Health care demands novel approaches in the diagnosis and treatment of patients as well as the delivery of high quality and safe patient care. The cost of quality is evident as demonstrated by pay-for-performance and the financial penalties implemented in 2008 by the Centers for Medicare Services (CMS). Quality measures are one of the methods used to gauge how well a health care organization provides evidence based standards of care that have been shown to result in improved clinical outcomes for patients. Today, many organizations face challenges with decreasing congestive heart failure patient’s length of stay. The role of the DNP is instrumental in the coordination of care involving combined efforts from various stakeholders, leading to better patient outcomes and system performance. The right blending of technology and health care delivery is an important aspect in establishing a timely service delivery that caters for patients’ self-centeredness.
This discussion presents the quality practice issues for decreasing length of stay for congestive heart failure patients through the analysis of the benchmarking process, describing the tools applied and the analysis results of real time data resulting in various options or solutions (Duffy, Kohers & Sower, 2007).
Background and Context of the Practice Issue
Through benchmarking of data, Baptist Medical Center identified that congestive heart failure patients had an average lengths of stay of half-day longer than patients did in comparable hospitals as reported in Premier’s Comparative Database (Birk, 2012). Baptist Medical Center should Adopt telemonitoring devices for CHF patients to enhance timely delivery.Telemontoring is important in gathering CHF patients’ data on a daily, consistent and automated manner. The system uses a wireless gateway device to capture important patients’ data such as weight, blood pressure, level of oxygen in the blood and ensure real-time monitoring of the CHF patients to enhance timely medication. Around the clock access of CHF patients’ data can greatly boost the caregivers’ delivery of service to the patients, which will enhance the recovery process. The implementation of the above model at Baptist Medical Center to decrease CHF patients’ length of stay is a strategic move in enhancing timely service delivery in the center (Louis, Turner, Gretton, Baksh & Cleland, 2003). When implemented in a hospital, this model involves the integration of a staged intervention to ensure there is compliance to the benchmarking standards (Beauregard, McDermott& Mikulak, 2009). On a real time basis, the patient is in a position to monitor his/her condition and relay important information to appropriate personnel. This is important in enhancing timely service provision for CHF patients (Stone & Hoffman, 2010).
Theoretical Underpinnings of Change for the Proposed Quality Initiative
Telemonitoring Model for the Quality Improvement Project
Any change process faces opposition. Thus, appropriate strategy is essential in underpinning the proposed change implementation. Kurt Lewin theory is appropriate in guiding the implementation of telemonitoring process at Baptist Health Center. The theory entails three fundamental steps, which include unfreezing stage that involve surveying the state of the existing method, identifying areas of failure and establish why change should take place. The survey of Baptist Health Center showed that the center suffers from delay in the duration of stay for CHF patients. Therefore, a change is essential to ensure delivery of timely services to enhance patients’ satisfactions. The change process will entail effective communication to create awareness for the impending change process. This will be important in preparing all concerned stakeholders (CHF patients and hospital personnel) about the need and importance of implementation of the telemonitoring process in the center. To facilitate the success of the process, the management will ensure support of the executives and try to address employees’ doubts, as well as concerns to create a positive perception for the change process. The next phase is the change stage. At this stage, the management should identify a special group to assign the role of overseeing the change process.
The group should involve all the heads of all the departments. The heads should explain to their respective members the benefits of adopting the telemonitoring process, as well as explaining to them on how the change process will affect everyone. The group should make sure that every concerned stakeholder gets proper assistance. The group should formulate short term and long-term goals, reward, and celebrate accomplishment of every goal as a motivational for reinforcing the change process. The final stage is the refreezing stage that comes after successful implementation of the telemonitoring process. At this phase, the team overseeing the change process should identify what supports the process and what restrains sustainability of the change process and act accordingly. During the refreezing stage, the management makes sure to address essential issues to sustain the change process, which entail; offering supportive leadership, reward, establish feedback systems, as well as adapting the Baptist Health Center structure accordingly, to accommodate the changes implemented. In addition, the managements should ensure training of appropriate stakeholders, as well as keeping the communication open to enhance sustainability of the change process (Kritsonis, 2005).
The Root Cause Analysis (RCA) (Occurrences drawn from the change process)
Baptist Medical Center applied RCA in enhancing the understanding of the CHF practice issue. The initial principles of RCA were applied to achieve an understanding of the actual cause of increased LOS for CHF patients and identification of the cause and effect relationship. This was achieved by focusing on the processes that take place from the time a CHF patient is admitted to the time a CHF patient is discharged from the hospital. Through data collection, the Baptist Medical Center team was able to realize their CHF readmission rates are below benchmark for two out of three DRG’s and the readmission rate for DRG293 is slightly higher (Latino, Latino & Latino, 2011). It was also found that there were no none-value added steps in their processes but there were nine delays identified. A Pareto chart was utilized to graphically show the relative importance of causes and defects of the nine delays found in the practice issue. This allowed the team to focus on the more significant opportunities for process improvement that had the greatest cumulative effect (Donaldson, 1991).
Resources Required For the Organizational Systems Change
Organizational systems change requires a large range of investment on resources. These range from qualified personnel, structural inputs as well as monetary investments (Cummings & Worley, 2009). There is need to employ qualified and skilled human resource with ability to comprehend and implement appropriate interventions for change processes. Additionally, both financial as well as structural requirements are vital to aid the process.
Baptist Medical Center utilized human resources to establish appropriate change processes. This included the addition of five concurrent Senior Data Quality Abstraction Specialist FTEs. There was deployment of concurrent coding in partnership with the Abstraction Specialists. This allowed for the identification and communication of potential Core Measure patients who met pre-selected criteria. Furthermore, employment of the Advanced Practice Role played an instrumental part in implementation of the change process. Collaboration of ideas for tracking potential CHF patients real-time to capitalize on opportunities to intervene in providing timely essential care was important in the success of the implementation process. Because of this real-time process, these driving forces have considerable impact on CHF compliance and outcomes (Hines, Yu & Randall, 2010).
Proposed Evaluation Method (S)
Data collection involving both qualitative as well as quantitative analysis techniques was applicable for this process. Process monitoring was critical in enhancing this initiative. Furthermore, design or reporting tools for progress reports as well as measuring of potential indicators and deliverables will help in monitoring as well as assist in verifying the real time empirical data derived from patient support medical equipment (Institute of Medicine, 2006).
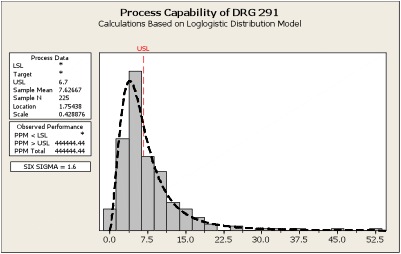
Analysis and presentation tools used involved statistical methods, which presented a positive performance. This was considering cost effectiveness and efficiency. Baptist Medical Center applied qualitative data findings to a FMEA model to anticipate, identify and prevent failures. The team was able to identify improvement opportunities, which if implemented during a rapid-cycle phase could greatly enhance performance. With rapid cycle improvements, a set of controls was important in evaluating the process improvements implemented and act as a guide for maintaining gains realized throughout the project. The process capability charts show the performance improvements implemented had positive effect on LOS of CHF patients. Process capability charts statistically measure the variation in the process. The first chart below indicates a 52-day LOS outlier. After implementation of process improvements, the “Improved” chart illustrates a reduced LOS process variation to approximately 10 days (Lewis & Passmore, 2011).
Similarly, questionnaires that contained open-ended questions were prepared to assists in assessing the patients’ recovery time, as well as the satisfaction of the new system in all the stakeholders affected. The distribution of questionnaires to appropriate stakeholders followed. Then there was coding and mapping of data corrected to generate appropriate inference. The qualitative results indicated that there was a great reduction in hospital stay for the CHF patients’, and all involved stakeholders were happy with the new implementation.
Conclusion
The right blending of technology and health care delivery is important in enhancing timely delivery. Baptist Medical Center faced a challenge in delivering timely services mainly to the CHF patients. However, by proper blending the technology and health care deliver, the facility recorded an improved performance in its service delivery. The new method made it possible for the caregivers to have real-time conditions of their patients that facilitate service delivery greatly. The method was highly appreciated by both the patients and hospital personnel because of its ability to cater for patients-centeredness and at the same time enhancing timely service delivery, which are essential IOM’s Dimensions of Quality. Along with continuous quality improvement initiatives, benchmarking remains a very important component of quality improvement within organizations such as healthcare providers. It is more critical to observe the positive effects of this process within health care provision areas. Data collections, as well as statistical approaches, are essential components of processes involved in benchmarking.
References List
Beauregard, M., McDermott, R., & Mikulak, R. (2009). The Basics of FMEA. (2nd ed.). NY, NY: Taylor & Francis Group.
Birk S. (2012). Reducing hospital readmissions. Healthcare Executive. 27(2), 17-24.
Cummings, T. & Worley, C. (2009). Organization development & change. Australia: South-Western/Cengage Learning.
Donaldson, M. (1991). Medicare–new directions in quality assurance: Proceedings of an invitational conference. Washington, DC: National Academy Press.
Duffy, J. A., & Kohers, G., Sower, V. E., (2007). Benchmarking for hospitals: achieving best in class performance without having to reinvent the wheel. Milwaukee, WI: American Society for Quality.
Hines, P., Yu, K., & Randall, M. (2010). Preventing heart failure readmissions: is your organization prepared? Journal of Nursing Economics. 28(2), 74-86.
Institute of Medicine (U.S.). (2000). Crossing the quality chasm: a new health system for the 21st century. Washington DC: National Academy of Sciences.
Kritsonis A. (2005).Comparison of Change Theories. International Journal of Scholarly Academic Intellectual Diversity. 8, 1, 145-167.
Latino, R., Latino, K., & Latino, M. (2011). Root cause analysis: Improving performance for bottom-line results. (4th ed.). Boca Raton, FL: Taylor & Francis Group.
Lewis, S. & Passmore, J. (2011). Appreciative Inquiry for Change Management: Using AI to Facilitate Organizational Development. London: Kogan PAGE.
Louis, A., Turner, T., Gretton, M., Baksh, A., & Cleland, J. (2003). A systematic review of telemonitoring for the management of heart failure. The European Journal of Heart Failure, 5, 583–590.
Stone, J., & Hoffman, G., (2010). Medicare Hospital Readmissions: Issues, Policy Options and PPACA. Congressional Research Service.