- Introduction
- The Problem and Outcomes for Older People
- Risk Factors for Falls
- The Use Of Self-Assessment Checklists
- Health Improvement Recommendations: Exercises
- Health Improvement Recommendations: Assistive Devices
- Health Improvement Recommendations: Lifestyle
- Helpful Resources and Links
- References
Introduction
This brief lecture is designed for community-dwelling people older than 65 years old and aimed at increasing their awareness of falls and effective fall prevention programs. I will provide some information about the size of the issue and risk factors. However, the major focus will be on prevention strategies, which is the most relevant aspect for you. I would like to note that I will employ such teaching strategy as the collaboration because I want to really engage you in the discussion and reflection on the matter. This approach implies the discussion and sharing ideas, concerns, fears, and emotions regarding different facets of the problem.
The Problem and Outcomes for Older People
Falls are a common health issue among the elderly that leads to serious negative outcomes for this population (Grossman et al., 2018). It has been estimated that almost 30% of older Americans fall each year. As a result, approximately 10 million falls result in medical care and patients’ restricted activity. The problem is rather huge as thousands of people die annually. For instance, 33,000 people died in 2015, which is a catastrophic trend.
Risk Factors for Falls
However, the problem is preventable, and talking about it is one of the effective solutions. By understanding risk factors, you will be able to estimate if your chances of falling are increasing. So, if for some reason, you have unmet medical care needs, your chances to fall grow (Marrero et al., 2019). Older people with depressive symptoms are prone to falling as well. The history of previous falls is associated with high risks of new incidents. Being male and older than 85 is another predictor of falls. Therefore, it is critical to pay specific attention to the areas mentioned above.
The Use Of Self-Assessment Checklists
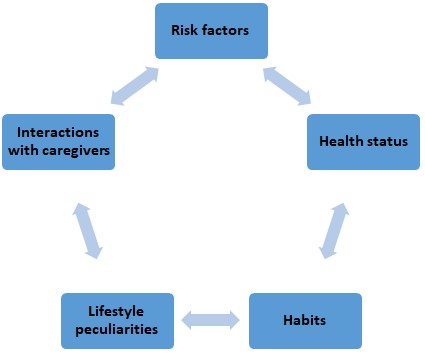
Although the evaluation of risks may seem a difficult task, it can become effective and even easy if self-assessment checklists are utilized (Marrero et al., 2019). These checklists often include a number of areas to consider. These include the reflection on risk factors and your health status, as well as habits and the peculiarities of your lifestyle. Self-assessment tends to have questions regarding your addressing healthcare professionals and the way you interact with your close ones. Clearly, when you complete such assessment forms, you have to be sincere and precise, which will help you estimate the chances of new falls effectively. A link to an effective assessment form will be provided at the end of the lecture. Have you tried such a prevention technique? If so, was it effective? Why or why not?
Health Improvement Recommendations: Exercises
A sufficient amount of exercise is another preventive strategy that has proved to be effective. Numerous researchers stress that exercise-based programs lead to the reduction of falls, improved balance, increased activity, and better psychological and emotional states (Grossman et al., 2018). Such options as dancing, yoga, tai-chi, gardening, and walking are some of the most effective preventive measures. It is also noteworthy that such programs are popular among older people, so you are also welcome to discuss this prevention tool efficiency.
Health Improvement Recommendations: Assistive Devices
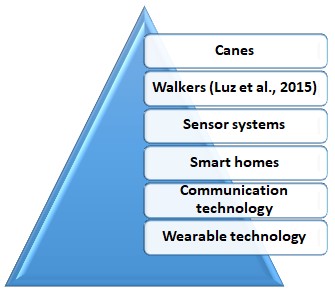
In addition to assessment checklists and exercise, the use of assistive technology is a helpful solution. Canes and walkers have been common instruments that considerably reduced the negative outcomes (Luz et al., 2015). At that, information and communication technology (ICT) is gaining momentum (Mackenzie & Clifford, 2018). Smart homes, wearable technology, and sensor systems are becoming more available, which leads to their increasing use (Chabot et al., 2019). Communication is one of the key aspects of effective program implementation and fall prevention. By means of their cell phones, older people can contact their caregivers and let them know about their health status, emotional state, or any other aspect.
Health Improvement Recommendations: Lifestyle

Older people often forget about the relevance of a specific lifestyle and the need to change some habits (Mackenzie & Clifford, 2018). You should make sure that you eat a healthy diet and have no bad habits. Be active, do exercise, and have a hobby, which will help you to be more physically and emotionally fit. You should be responsible and remember that the way you live will affect the way you move. Of course, you should maintain social contacts and participate in various activities that are held in your community.
Reflect on bad habits you should abandon. Do you know about any programs or incentives for older people that are available in your community?
Helpful Resources and Links
- Healthy People 2020. Web.
- Self-assessment checklist. Web.
- Some exercise. Web.
References
Chabot, M., Delaware, L., McCarley, S., Little, C., Nye, A., & Anderson, E. (2019). Living in place: The impact of smart technology. Current Geriatrics Reports, 8(3), 232-238.
Grossman, D. C., Curry, S. J., Owens, D. K., Barry, M. J., Caughey, A. B., Davidson, K. W., Doubeni, C. A., Epling Jr, J. Kemper, W. A. R, Krist, A. H., Kubik, M., Landefeld, S., Mangione, C. M., Pignone, M., Silverstein, M., Simon, M. A., & Tseng, C.-W. (2018). Interventions to prevent falls in community-dwelling older adults. JAMA, 319(16), 1696-1704.
Luz, C., Bush, T., & Shen, X. (2015). Do canes or walkers make any difference? Nonuse and fall injuries. The Gerontologist, 57(2), 211-218.