Introduction
The rapid advancement of information technology and data preservation and storage techniques could not go unnoticed for the healthcare field due to the professional area’s demanding requirements regarding patient data flow, management, and storage. Electronic medical record (EMR) systems are aimed at taking medical history management practices to the next level, thus guaranteeing patient safety, reducing medication errors that stem from poor information sharing and coordination, and facilitating medication prescription processes. Healthcare providers in the United States develop EMR solutions or adopt ready-made solutions from vendors for clinical tasks at an increasing rate since the departure from paper-based medical records guarantees more security in case of catastrophic events and natural disasters. At the same time, the need to hold personal accountability for individual healthcare data entries ensures providers’ responsibility and carefulness during data collection and management endeavors. This report explores the uses of EMR applications by discussing the case of an emergency department (ED) of Hospital X.
Organization Information
Background Information: Organization Type and the HIT System
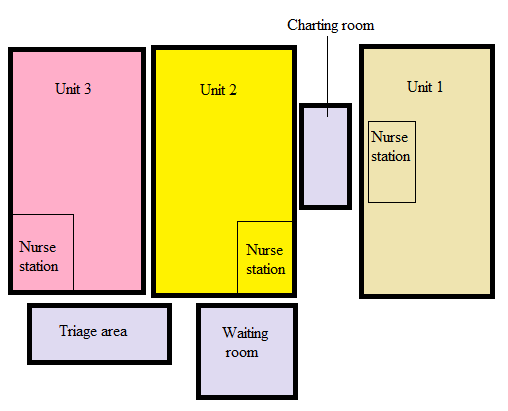
The selected healthcare organization is the ED of a medium-sized acute care hospital in the United States. In a brief interview by phone, the representative of the chosen healthcare facility agreed to discuss the EMR system and basic clinical challenges leading to its adoption. Due to the fear of reputational losses and patients’ concerns, the organization wishes to be referred to as Hospital X, so no identifiable information can be disclosed. The ED of Hospital X is a six-area facility with one charting room where ED doctors work, the ED waiting room, the triage area where the triage nurse evaluates new patients, and three separate units for treating conditions of different severity (J. Doe, personal communication, April 20, 2021). Figure A1 demonstrates a simplified scheme of the department that has been created for this assignment. The health information technology (HIT) system that Hospital X currently uses is EpicCare EMR with special features for ED clinical practice. The solution has been purchased from Epic, a well-known healthcare software developer with a positive reputation.
The HIT System’s Purpose
Hospital X has been using the aforementioned EMR solution for the purpose of optimizing patient evaluation processes and adding to each client’s safety. The goals of increasing the speed of clinical decision-making and keeping track of patients’ physical condition without any data losses are also critical. In terms of safety, similarly to any facility that deals with patients suffering from somewhat unpredictable conditions, Hospital X values accuracy in decision-making related to medication prescription and emphasizes measures to eliminate the risks of mistakes, including dosage delays, missed doses, wrong administration routes, and so on (J. Doe, personal communication, April 20, 2021). Therefore, the EMR use by the department’s clinical staff mainly serves clinical purposes.
Reasons for Development and Need Determination Practices
For the selected organization, the need for a reliable EMR system from a trustworthy vendor arose a few years ago. Prior to purchasing a solution from Epic Systems Corporation, the ED was using another, more primitive EMR system that did not have features that would best fit the provision of emergency services and sometimes failed to display recently entered admission data correctly (J. Doe, personal communication, April 20, 2021). The most concerning aspects of the former system’s operation were the instances of medical record duplication; also, an insufficient operation speed was not aligned with the specifics of emergency care (J. Doe, personal communication, April 20, 2021). Because of slow operation and interface-related inconvenience, there have been instances of documentation errors, such as uploading incomplete information on ED events for individual patients or uploading information in the wrong files (J. Doe, personal communication, April 20, 2021). These needs were determined based on staff members’ persistent complaints about software’s quality and inadequate time expenditures related to patient data entry activities, and an anonymous survey was also implemented to make the decision to start EMR software replacement.
System Selection
The predetermined needs, such as convenience, reduced data input challenges, and data management features developed for ED service providers, required Hospital X to engage in the vendor selection process, which resulted in choosing EpicCare EMR. The organization contacted a few prominent vendors in the market, including Epic Systems Corporation, Medhost, and Cerner Corporation, and evaluated their offerings for ED physicians and nurses (J. Doe, personal communication, April 20, 2021). Epic has become one of the most popular EMR software vendors in recent years, partially due to vast customization and module selection opportunities, as well as compliance with the Health Insurance Portability and Accountability Act enacted in 1996 (Tan et al., 2017). Some factors that led to this choice include Epic Systems Corporation’s professional reputation, positive feedback from organizations, including ED services, interface design’s relative simplicity, ease of use, and HIPAA compliance (J. Doe, personal communication, April 20, 2021). Other EMR options were rejected despite being a bit more affordable.
The Management of the HIT System
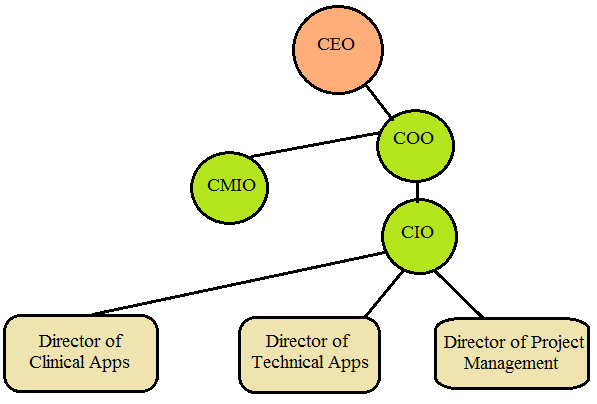
At Hospital X, the selected HIT application is managed by a team of people. During the implementation stage, the EMR implementation team, including an IT lead, a nurse lead, and an implementation manager, was responsible for installation and initial teaching processes (J. Doe, personal communication, April 20, 2021). These individuals held different positions in the facility’s administrative structure, including a senior critical care nurse and a chief medical informatics officer. As of now, the hospital’s CMIO (a physician with health IT training) and a director of clinical applications fulfill most of the system monitoring and management tasks. As for their administrative hierarchy positions, the CMIO reports to the IT department’s chief operating officer and serves as a liaison between the clinical staff and IT staff, whereas the director of clinical applications oversees applications’ use and reports to the department’s chief information officer (see Figure A2). Therefore, although the EMR system has not been developed by the organization, there is a range of professionals that keep track of its clinical implementation to discover technical issues in good time and prevent disruptions to the well-established patient management processes.
Information System Application Design and Development
Decision-Making and End-Users’ Involvement
During software provider evaluations, purchase planning, and installation processes, decisions at Hospital X were made by the interprofessional EMR team created for that purpose. The director of clinical applications and the CMIO were specifically active during vendor selection and presented their analysis of EMR options and vendor comparison results to the hospital’s chief executive officer for approval (J. Doe, personal communication, April 20, 2021). In collaboration with clinical staff, these stakeholders continue to make decisions regarding the need for requesting technical support from the vendor (J. Doe, personal communication, April 20, 2021). The EMR application’s end-users, such as ED physicians, anaesthesiology professionals, and nursing staff, impacted the decision-making process by filling out a brief form that encouraged them to outline expectations from a new system.
How Individuals Are Trained to Use the EMR System
End-user training is a critical part of success in the post-implementation stage, and Hospital X resorts to training resources from the vendor to facilitate skill improvement in ED physicians and nurses. As per research, numerous training-related factors, including educational efforts’ timing, the consideration given to users’ needs, and access to on-site technical support, affect the extent to which EMR applications’ potential is realized (Sharp et al., 2017). Also, it has been demonstrated that professionals in diverse clinical settings have vastly different EMR training needs, which calls for training interventions based on the specifics of one’s clinical role (Lopez et al., 2018). Hospital X incorporates this requirement by supporting a specific training program for ED nurses.
The presence of users’ adequate IT and EMR skills is a critical priority for the organization. Hospital X encourages staff members that are to support the operation of the EMR system to complete Epic EMR training courses and certification tests offered by Epic Systems Corporation and sponsors these continuing education endeavors, and these activities require considerable financial contributions (J. Doe, personal communication, April 20, 2021). Also, e-learning methods are widely implemented to develop EMR use skills in ED care staff, and Hospital X collaborates with a medical university that offers a 15-module online program for emergency care nurses (J. Doe, personal communication, April 20, 2021). Each module covers one specific Epic EMR-related activity, such as managing orders or working with flowsheets, and includes educational content in the forms of lectures, video demonstrations, readings, and lab sessions with assignments that measure knowledge and skills (J. Doe, personal communication, April 20, 2021; Randhawa et al., 2020). Finally, right after switching to Epic EMR, Hospital X concluded agreements with certified Epic-credentialed trainers offering group training on data entering, security measures, order placement, patient evaluation, and available functions.
Security Issues and Supporting Legally Sound Healthcare Records
Hospital X instructs employees on how to deal with potential security issues. Firstly, in the organization’s internal training materials, every end-user in the ED is introduced to basic security measures, such as using reliable password storage solutions and logging out or securing computers with passwords to prevent unauthorized access to personal medical data (J. Doe, personal communication, April 20, 2021). There are information security signs near all computers to remind staff members of the key information security practices.
To continue, any effective EMR system, including Epic’s products, must be protected. Such reliable systems utilize a series of sophisticated security policies against cross-site scripting attacks and SQL injections, and protection is often achieved by means of secret tokens and other techniques (Adamu et al., 2020). Additionally, Epic Systems Corporation (2021) also accepts reports of security concerns from clients, so Hospital X’s employees can seek official support from the company in case of security threats. Epic’s EMR and EHR software, as well as Epic’s telehealth applications, incorporate the HIPAA security rule and are mentioned in the list of HIPAA compliant systems produced by the organization of the same name (J. Doe, personal communication, April 20, 2021; Hildrew et al., 2020). Adequate privacy protection measures contributing to this recognition support the generation of legally sound healthcare records.
Funding, Budget Management, and Organizational/Political Issues
The implementation of Epic’s EMR system required Hospital X to make substantial investments. Even with thorough financial planning, it is not uncommon for actual EMR deployment costs to exceed the formerly anticipated budget (Papalou, 2020). The initial funds for purchasing EpicCare EMR came from the hospital’s patient and nonpatient revenues and a local non-bank lender; the organization also used a deferred payment option from the vendor (J. Doe, personal communication, April 20, 2021). The organization’s accounting department staff and the chief financial officer take responsibility for EMR-related cost assessment and budget management activities (J. Doe, personal communication, April 20, 2021). Vendor selection and installation took place before recent systems-level challenges, such as the COVID-19 outbreak in the U.S. (J. Doe, personal communication, April 20, 2021). Thus, no specific political or organizational issues have impacted Hospital X’s purchasing decision and the plan to shift to another EMR application.
Planned/Unplanned Downtime Arrangements and Scheduling of EMR System Upgrades
Downtime events and application upgrades also affect end-users’ experiences. Hospital X provides staff members with internal documents with detailed instructions regarding EMR use during planned downtime. Before the downtime event, Epic’s Shadow Read Only (SRO) operating mode should be used to view patient data and make sure that it has been saved properly, and manual patient information forms with special labels are made available (J. Doe, personal communication, April 20, 2021). Patient data entry instructions after the end of the event depend on some factors, including downtime duration and whether the professional completing manual forms had to hand them over to the next shift, but all data on assessments are to be entered as soon as possible (J. Doe, personal communication, April 20, 2021). Similar policies exist for unplanned downtime events, with rapid shifting to paper-based documentation and informing the IT department about the error as the key activities (J. Doe, personal communication, April 20, 2021). For upgrade planning, Hospital X collaborates with the vendor to explore new data management options and evaluates staff members’ feedback on documentation-related challenges (J. Doe, personal communication, April 20, 2021).
Changes Related to Healthcare Reform/Legislation and Suggestions
EpicCare EMR appeared in the medical software market in the early 1990s, years before Epic’s tremendous popularity, and it was among the first Windows-based applications that could reduce excessive paperwork (J. Doe, personal communication, April 20, 2021). Healthcare reforms that could have influenced Epic’s EMR software include the Health Information Technology for Economic and Clinical Health act of 2009 that called for increased HIT adoption. After 2009, Epic announced the introduction of new features and data processing methods, including voice recognition and patient portal use (J. Doe, personal communication, April 20, 2021). Increases in the number of operating systems supporting EpicCare and the introduction of access logs that record the time of access, users, and devices from which the system is entered supports providers’ accountability for care outcomes and makes the product more flexible for use (Tai-Seale et al., 2017). To some degree, new features may serve the purpose of promoting the meaningful use of HIT applications in clinical settings.
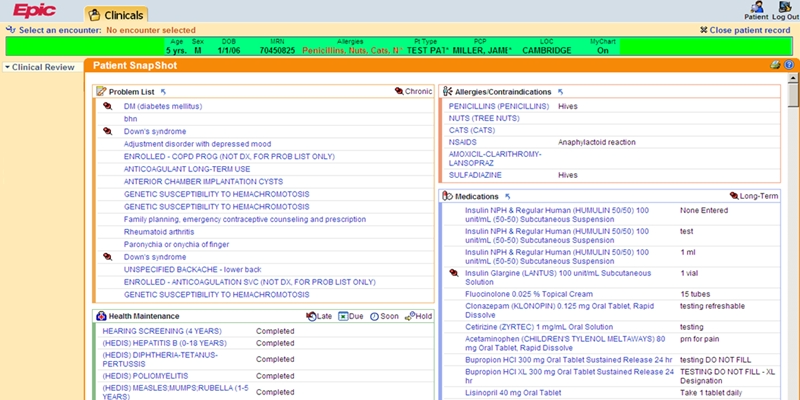
As for suggestions for improvement, further encouragement of EMR and EHR use in small-to-medium hospitals might require the reconsideration of Epic’s software pricing policies since EpicCare remains relatively expensive. Also, there are minor disadvantages noticed by some end-users, such as color themes hurting the eyes (see Figure A3), non-intuitive design, or the need for too many clicks to fulfill basic tasks (J. Doe, personal communication, April 20, 2021). To maximize users’ positive experiences with EpicCare, thus promoting the further achievement of plans outlined in the HITECH, it might be critical to offer design-related updates.
Innovative Aspects of the System
The Application and Technology Innovations
The EMR system selected by Hospital X makes use of some relatively recent functions, such as voice recognition. Particularly, clinicians have the opportunity to install Dragon Medical speech-to-text software and integrate it with EpicCare EMR, but not all ED clinicians regard this option particularly safe and easy to use because of noise levels (J. Doe, personal communication, April 20, 2021). As per current research, speech recognition technology (SRT) in clinical documentation is considered a promising method of optimizing the workload on nurses and enabling the latter to increase the amount of time devoted to direct care activities (Joseph et al., 2020). In a systematic review of ten studies that test diverse SRT applications and devices, Joseph et al. (2020) report that SRT clinical use is associated with increases in nurses’ documentation-related productivity and the accuracy of patient records. However, SRT in HIT applications may involve disadvantages, including financial burden and the need for employee training (Joseph et al., 2020). If implemented without due training, SRT can possibly lead to the loss of patient assessment data.
Recommended Innovations and Methods to Promote EBP and Efficiency
There are some innovations that could be recommended to support evidence-based practice in Hospital X’s case and benefit the organization. Firstly, modern peer-reviewed literature in the urethral surgery field offers the innovative uses of the Epic EMR platform that Hospital X might find helpful. Particularly, Javier-DesLoges et al. (2019) developed and tested a methodology for preventing ureteral stent-related adverse events by logging and keeping track of data on urethral stent insertion and removal to monitor potential stent loss cases and eliminate related mistakes. Apart from collecting data on stent placement, the method involves measures for the automated reporting of stents implanted for a few months and monthly reviews of patient data reports (Javier-DesLoges et al., 2019). Although stent loss cases are relatively uncommon, the methodology might serve as a reference model to prevent more frequent mistakes that are more likely in Hospital X’s care environment.
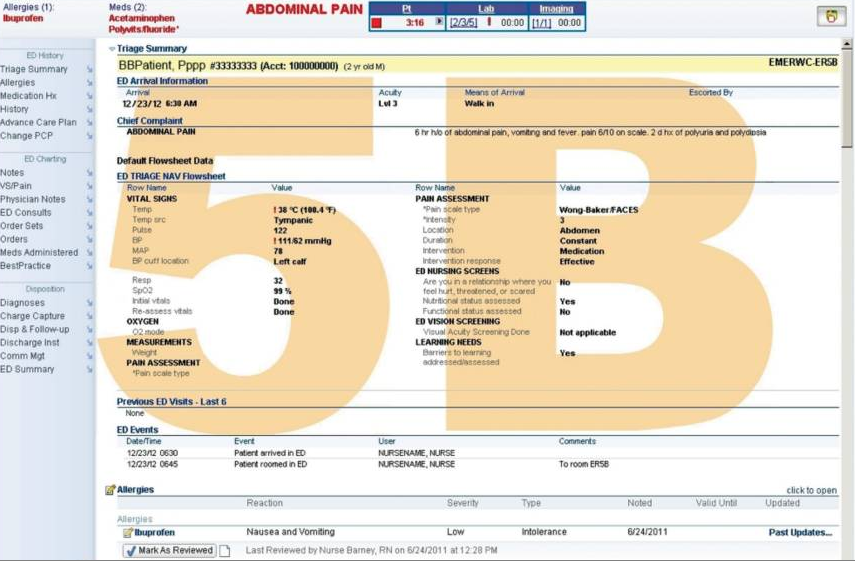
Another customization-related EMR software innovation that could be recommended to Hospital X refers to strategies to prevent medication mistakes due to constant distractions and the risks of patient confusion affecting ED clinicians’ behaviors. The measure that can support error prevention in EDs is the introduction of large watermarks with the patient’s room number on the patient encounter screen in Epic EMR tested by Yamamoto at one ED in Honolulu (Grissinger, 2018). As Figure A4 demonstrates, the measure offers instant and uninterrupted access to patient room number information, which can reduce the time needed to check the correctness of medication orders and exclude confusion between two patients in different rooms that have similar names.
Conclusion
In summary, based on Hospital X’s case, EMR solutions from Epic Systems Corporation remain a popular choice among healthcare providers, which deals with their regulatory compliance, reliability, and operability. Even in the case of purchasing ready-made EMR systems, hospitals are required to make numerous important decisions, including assigning the responsibility for meetings with vendors and clinical staff, evaluating software options’ financial feasibility, analyzing costs, determining education needs, planning downtime procedures, and so on. Considering this, despite bringing positive outcomes and ensuring hospitals’ ability to stay current, HIT implementation in clinical settings is a complicated process involving challenges.
References
Adamu, J., Hamzah, R., & Rosli, M. M. (2020). Security issues and framework of electronic medical record: A review. Bulletin of Electrical Engineering and Informatics, 9(2), 565-572.
Epic Systems Corporation. (2021). Reporting a potential security vulnerability or concern. Web.
GetApp. (n.d.). EpicCare EMR overview. Web.
Grissinger, M. (2018). Selected medication safety risks that can easily fall off the radar screen. Pharmacy and Therapeutics, 43(9), 521, 567. Web.
Hildrew, D. M., Pang, K., & Faden, D. (2020). Otolaryngology in the time of COVID: An overview of common open-source telemedicine platforms. Laryngoscope Investigative Otolaryngology, 5(5), 839–845.
Javier-DesLoges, J. F., Johnson, K. K., Kenney, P. A., & Motamedinia, P. (2019). Novel use of the Epic electronic medical record platform to identify lost ureteral stents. Journal of Endourology, 33(10), 858-862. Web.
Joseph, J., Moore, Z. E., Patton, D., O’Connor, T., & Nugent, L. E. (2020). The impact of implementing speech recognition technology on the accuracy and efficiency (time to complete) clinical documentation by nurses: A systematic review. Journal of Clinical Nursing, 29(13-14), 2125-2137. Web.
Lopez, C. A., Omizo, R. K., & Whealin, J. M. (2018). Impact of a tailored training on advanced electronic medical records use for providers in a Veterans Health Administration Medical System. JAMIA Open, 1(2), 142-146. Web.
Papalou, A. (2020). Proposed information system towards computerized technological application – recommendation for the acquisition, implementation, and support of a health information system. International Journal of Communication and Computer Technologies, 8(2), 1-4. Web.
Randhawa, G. K., Shachak, A., Courtney, K. L., & Kushniruk, A. (2020). Effective design, development, and evaluation of video tutorials for electronic medical record training. ACI Open, 4(1), e69-e82. Web.
Sharp, K., Williams, M., Aldrich, A., Bogacz, A., Denier, S., & McAlearney, A. S. (2017). Conversion of provider EMR training from instructor-led training to eLearning at an academic medical center. Applied Clinical Informatics, 8(3), 754-762. Web.
Tai-Seale, M., Olson, C. W., Li, J., Chan, A. S., Morikawa, C., Durbin, M., Wang, W., & Luft, H. S. (2017). Electronic health record logs indicate that physicians split time evenly between seeing patients and desktop medicine. Health Affairs, 36(4), 655-662. Web.
Tan, B. T., Fralick, J., Flores, W., Schrandt, C., Davis, V., Bruynell, T., Wilson, L., Christopher, J., Weber, S., & Shah, N. (2017). Implementation of Epic Beaker Clinical Pathology at Stanford University Medical Center. American Journal of Clinical Pathology, 147(3), 261-272.
Yamamoto, L. G. (n.d.). Patient encounter screen with room number watermark [Image]. Web.
Appendix A