Hypertension is a prevalent lifestyle disease affecting approximately 42% of the adult population. According to WHO, high blood pressure (HBP) is a significant cause of premature deaths globally (Arrendondo et al., 2017). For that reason, curative and preventive measures target to reduce its prevalence by 33% by the year 2030. The high-risk population includes the aged, pregnant women, obese individuals, and physically inactive people (Beckie, 2017). Specific concepts like health disparities, ethical considerations, human rights, and health determinants are fundamental in discussing hypertension. All these factors bear a direct or indirect relationship with this condition.
Health disparities in hypertension are primarily associated with race and socioeconomic status. According to Arrendondo et al. (2017), the primary financial disparities contributing to poor HBP control are substandard insurance cover and lack of (limited) access to healthcare. Low-income individuals cannot afford antihypertensive therapy and thus have higher mortality rates (Arrendondo et al., 2017). This data is instrumental in informing measures to assist populations in this category. Race and ethnicity also contribute to significant differences in hypertension prevalence due to genetic disparity, diversity of social factors, variation in response to therapy, and dissimilarity in cultural-specific treatments (Zanchetti,2018).
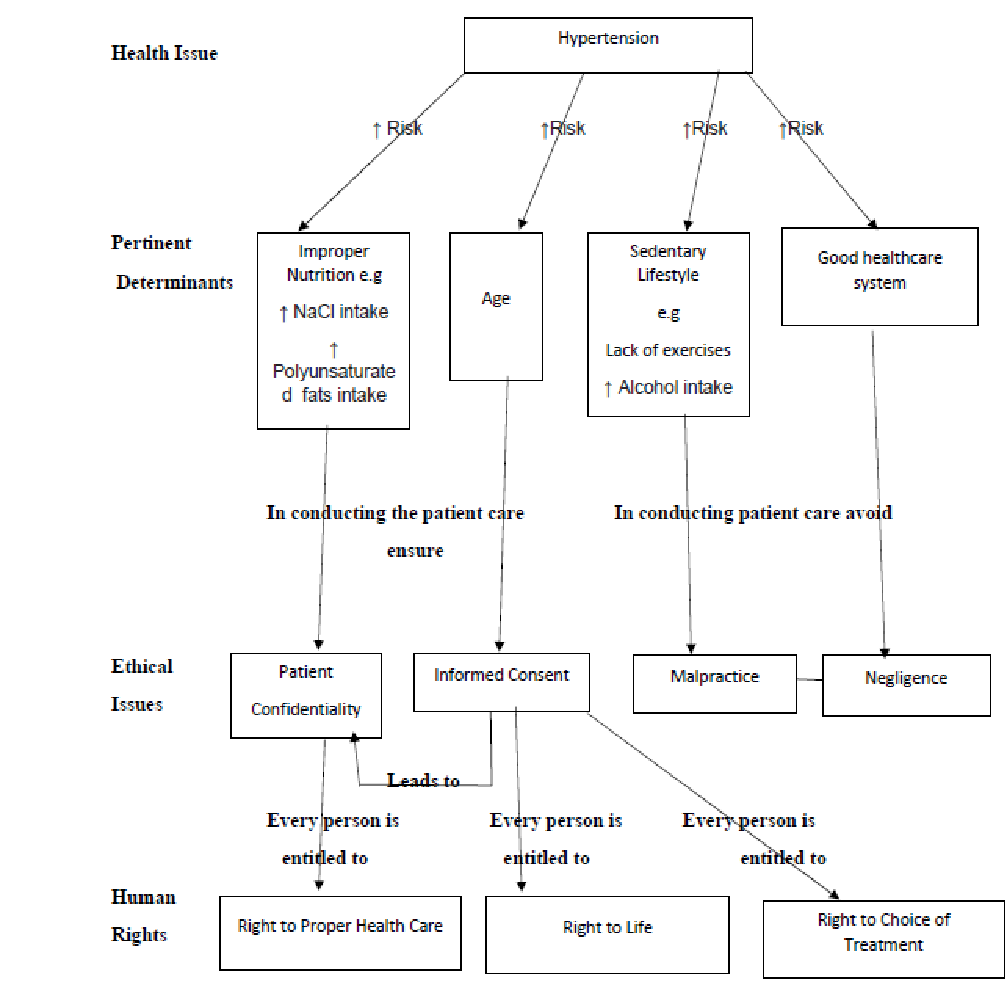
Multiple factors determine the onset and progression of high blood pressure. They can be classified based on their relation to ethical issues and human rights. Determinants of health in the first group include improper nutrition, excessive salt intake, and increased consumption of polyunsaturated fats (Beckie, 2017). These risk factors require the practitioner to educate the patient on high-risk behaviors associated with hypertension. In doing so, the physician must observe medical ethics by maintaining doctor-patient confidentiality. Discretion can also be upheld by safeguarding the patient’s medical records from unauthorized personnel. Through educating the patient, the practitioner impacts knowledge on preserving or restoring health; thus, observing the human right to health.
The second category of health determinants in hypertension comprises age. Elderly populations are typically associated with HBP primarily due to existing atherosclerosis (Arrendondo et al., 2017). Complications are common in these patients, and issues about euthanasia and choice of treatment may arise. Medical ethics direct that the practitioner protects the patient’s right to autonomy. The physician should also lucidly explain to the patient the best treatment options available to obtain informed consent. The healthcare practitioner honors the right to life by administering medication to preserve life (beneficence).
The third group of health determinants constitutes sedentary lifestyle (physical inactivity) and chronic alcohol consumption. Patients who develop hypertension due to these factors may be overlooked as some practitioners perceive them “responsible” for their ill health (Arrendondo et al., 2017). Each physician is duty-bound to provide healthcare services to those in need; therefore, practitioners should not disregard patients for whatever reason.
Negligence leads to litigations, which subsequently diminish healthcare resources as most reserves are directed towards fighting lawsuits. The fourth group of health factors comprises a sound healthcare system that reduces the risk of hypertension. Optimal healthcare services are crucial in reducing the prevalence of high blood pressure (Beckie, 2017). Recent studies reveal that some patients receive better services than others due to their economic status. This is unethical as physicians ought to ensure justice by treating all patients alike and ensuring fair allocation of resources. Practitioners should also avoid malpractice while conducting patient care.
References
Arredondo, A., Recaman, A. L., & Azar, A. (2017). Socioeconomic determinants and health disparities in relation to hypertension in middle-income countries. American Journal of Hypertension, 30(4), 355–357. Web.
Beckie, T. M. (2017). Ethnic and racial disparities in hypertension management among women. Seminars in Perinatology, 41(5), 278–286. Web.
Zanchetti, A. (2018). From risk factors to treatment of hypertension. Journal of Hypertension, 34(1), 1–2. Web.