Abstract
Hospital-acquired Pressure Injuries (HAPIs) are costly to the healthcare system and can be prevented. Due to the absence of an evidence-based prevention bundle for reducing the incidence of HAPIs, the project site experienced continued HAPIs in their patient population. The purpose of this quantitative, quasi-experimental project was to determine Rivera’s Pressure Injury Prevention (PIP) would impact HAPIs prevalence rate among critical care patients in a critical care unit in the Urban New York over four weeks. The healthcare quality improvement project was implemented in the western state critical care unit over four weeks. The caring nursing theory by Jean Watson’s was used to identify how Rivera’s PIP bundle could impact the HAPI incidence. Data on the impact of Riviera’s pressure injury prevention bundle was measured among critical care patients (n=64). The results were obtained through a t-test that indicated a high significance between the application of Rivera’s pressure injury prevention bundle and the reduction of pressure injuries.
Keywords: Hospital-acquired pressure injuries (HAPI), HAPI prevalence rates, and PIP.
Introduction to the Project
Hospital-acquired pressure injuries (HAPI) are a significant burden for healthcare organizations worldwide that negatively impact the quality of life of patients and their caregivers. The global prevalence of HAPI is almost 13%, while the incidence rate is above 5 per 10,000 patient days (Li et al., 2020). Most cases of HAPI are preventable; however, highly cachectic patients may develop pressure injuries despite the use of cushions for pressure distribution (Ricci et al., 2017). In addition to being a stressful event for patients, HAPI is also a formidable financial burden because most pressure ulcers develop as a secondary condition, requiring additional expenses (Mansfield et al., 2019). According to national estimates, the overall expenditure for treating patients with HAPIs is close to $11 billion (Padula & Delarmente, 2019). The HAPI prevalence in the 13-bed medical intensive care unit (MICU) in urban New York was reported to be 14%, which is higher than the national average. Therefore, this quality improvement project aims to determine how implementing evidence-based practices, specifically Rivera’s pressure injury prevention (PIP) bundle, can reduce the HAPI incidence in the 13-bed MICU.
Although many evidence-based methods were developed to address pressure ulcer development in hospitalized patients, HAPI’s national prevalence and treatment costs remain high. Approximately 2.5 million American patients in intensive care units annually develop pressure injuries that result in 60,000 deaths (Padula & Delarmente, 2019). The incidence rate of HAPIs in intensive care units varies from 14% to 42% (Anderson, 2018). Moreover, according to Padula and Delarmente (2019), the treatment cost for one pressure injury ranges from $500 to $70,000 because HAPIs lead to more extended hospital stays. The length of stay of patients with HAPI can increase by 14 days, thereby disrupting patients’ physical and emotional well-being (Ricci et al., 2017). Therefore, finding an effective intervention is critical for resolving multiple issues associated with HAPIs. Indeed, the exploration of this topic started in the nineteenth century, and the first intervention to prevent HAPIs was developed by Browning (Mansfield et al., 2019). Still, the approach that would eliminate a high HAPI prevalence problem has not been described yet.
Since various risk factors contribute to the development of HAPIs, introducing Rivera’s PIP bundle can address several issues simultaneously. The risk factors associated with the formation of pressure ulcers include older age, reduced mobility, poor nutrition, dehydration, reduced tissue perfusion, oxygenation, and medical devices placement (Romanelli et al., 2018). The primary function of Rivera’s PIP bundle is to recognize risk and prevent HAPI with appropriate interventions for high-risk patients. The intervention was developed by Rivera et al. (2020), whose methodology was based on assigning mediation depending on the severity of tissue damage. Specifically, patients with superficial HAPIs could receive a standard treatment plan, while those with deep pressure ulcers needed high-risk interventions (Rivera et al., 2020). The effectiveness of this approach was tested in an 11-bed critical care unit in one of the hospitals in New York City (Rivera et al., 2020). The results of the study demonstrated a seven-fold decrease in HAPI incidence in this department.
Chapter 1 presents background information regarding the problem of HAPIs in the literature and compares the information to the project site data. The problem at the project site is fully described along with the project’s purpose, clinical question, and explanation of how the work advances scientific knowledge. The chapter will also present data regarding the project significance, the rationale for choosing a specific methodology and a project design, definitions of terms, key assumptions, limitations, delimitations, and the summary.
Research Background
Pressure injuries have been a recurrent problem for the healthcare industry and, therefore, present historical data for consideration. The Joint Commission (2016) defines a pressure injury as localized skin and tissue damage caused by exposure to a medical device. Ricci et al. (2017) stipulate that the pressure ulcer prevalence was slightly lower than 15% in 1999; the 2009 International Pressure Ulcer Prevalence Survey reveals similar results. Li et al. (2020) also state that HAPI prevalence is approximately 12.8%, while its incidence rate is 5.4 per 10,000 patient days (p. 2). According to the World Health Organization [WHO] (2008), their prevalence rates are relatively similar across various nations, including 10% in the USA, 11% in Germany, 12% in Sweden, and 13% in Israel (p. 45). These statistical data reveal that HAPIs are a significant threat to quality health care that affect over 2.5 million individuals resulting in 60,000 deaths (Padula et al., 2019, p. 132). Rivera et al. (2020) also tested the effectiveness of their PIP bundle for reducing HAPIs in a New York critical care facility, thus, showcasing how hospital-related injuries are as much a local problem as they are a global issue. The HAPI prevalence rate in the urban New York project site’s medical intensive care unit was 14% in 2020, which was higher than the national rate. Consequently, this quality improvement project aims to investigate the scourge and determine if Rivera’s PIP bundle presents a feasible solution for HAPI prevention in the project facility.
Problem Statement
HAPIs negatively impact the quality of life of patients and their caregivers. Their high prevalence rates imply that they also incur huge financial costs for the health care sector. The situation is not different from our healthcare facility. Our organization has a thirteen-bed intensive care unit. The facility is almost always full throughout the year. As such, the organization registers HAPIs incidence rate of about fourteen percent. The incidence affects the facility in different ways. For instance, the hospital is forced to extend a majority of the HAPIs cases’ hospital stay by about ten days. The result of such is the growth of our facility’s annual expenditure by about five million. Moreover, maintaining patients in the facility while managing HAPIs cases denies the organization the chance to take of other needy patients. The issue thus amounts to significant loss of opportunity, whose cost amounts to about seven million dollars a year.
The point that the Medicare and Medicaid programs do not cater for HAPIs management leaves our organization with significant financial burden that needs intervention. Better still, one of our organization’s goals is to promote quick recovery among patients through the establishment and utilization of evidence-based interventions that make healing process easy and rapid. The point that the entity reports HAPIs cases implies substantial failure. That is why the institution is determined to eradicate the matter to not only save the high costs incurred, but also promote the quality of provided care. As such, the implementation of Rivera’s PIP bundle stands to impact HAPI incidence in our organization significantly. The present study thus seeks to investigate the effectiveness of the new intervention (Rivera’s PIP bundle) in solving the matter, by comparing the current HAPIs rate to that registered under the new intervention. The realized data will be compared to that recorded in critical care units in urban New York.
Purpose of the Project
The quality improvement project is to determine the impact of Rivera’s PIP Bundle on the HAPI incidence when compared to current practice among critical care patients in a 13-bed unit in urban New York. The independent variable, Rivera’s PIP Bundle, is an evidence-based assessment and intervention tool for mitigating HAPIs in patients. It delineates assessment, prevention, and mitigation strategies for both standard and high-risk patients. The bundle outlines varied interventions for the pressure ulcers depending on the level of risk the patient faces. The high-risk component includes more interventions such as dressing, turning, and positioning. Thus, it is a tool to help health care professionals standardize prevention of HAPIs and reduce their incidence.
The dependent variable, a HAPI incidence rate, was measured by the number of patients who developed pressure injuries due to medical devices during their hospital stays. Nurses are well-positioned to identify the condition and regularly updated their patient electronic health records (EHRs) about patients who developed them. Thus, the project site collected data about patients who developed HAPIs from the hospital’s EHR. HAPI incidence rate was useful for the indicating the impact of the quality improvement project. Lower incidence rates indicate an improvement in quality of care offered at the units and reduced costs of care.
Clinical Question
Our organization records a significantly high HAPIs rate of fourteen percent. The issue exposes the institution to numerous expenses amounting to millions of dollars a year. Other troublesome elements related to the high HAPIs incidence at the institution concerns the general perception of the quality of care offered. Padula et al. (2019) note that HAPIs prevalence in a healthcare facility partly implies an organization’s reduced quality of care. The argument, together with the recorded HAPIs incidences, contradicts our organization’s mission and vision statement. It is thus vital that the organization finds reliable interventions to resolve the matter before it gets out of hands. The entity believes that adopting PIP stands to cause the intended positive changes. “To what degree does the implementation of Rivera’s PIP bundle impact the HAPI incidence compared to current practice among critical care patients in a 13-bed unit in urban New York over four weeks?” is thus the present study’s guiding clinical question. The question sought to identify whether using Rivera’s PIP bundle is sufficient to reduce the HAPI incidence.
Advancing Scientific Knowledge
Scientific evidence indicates that HAPIs are a significant problem for health care. Ricci et al. (2017) and the 2009 International Pressure Ulcer Prevalence Survey reveals that that the pressure ulcer prevalence was slightly lower than 15% in 1999. Even though pressure injuries and their associated care costs have created immense problems for the entire healthcare industry, no improvement attempts have generated the required outcomes. Li et al. (2020) state that the HAPI prevalence is 12.8%, and the incidence rate is 5.4 for every 10,000 patient days (p. 2). These statistical data reveals a challenging situation in health care. Padula et al. (2019) support the claim stating that pressure injuries cause approximately 60,000 deaths among an affected population of over 2.5 million individuals (p. 132). The high prevalence, incidence, and mortality rates of HAPIs reveal a gap in care (Padula et al., 2019). There is insufficient literature that provides significant interventions for the prevention and treatment of HAPI.
The DPI project utilizes human caring nursing theory (Watson, 2018) to identify how utilization of PIP bundle can be associated with reduced HAPI incidence. Jean Watson (2018) proposes the theoretical framework by highlighting how to provide positive outcomes during human-to-human caring moments. She stipulates patients cannot be separated from the healthcare workforce, implying that a change occurs through nurses. Among the theory’s constructs are health, nursing, human being, and society (Watson, 2018). Its assumptions are also based on the need for interpersonal relations within care settings that promote growth and autonomy. Cheng et al. (2020) also note that the occurrence of HAPIs indicates a gap in the care process as patients who visit hospitals acquire secondary diseases that decrease their mortality, morbidity, and quality of life. The scholars insist that nurses ought to intervene in the process to provide care that holistically treats the individual and promotes their growth and autonomy. As such, the Cheng and his colleagues’ work and theory drives the present project’s endeavor to provide a solution to the rising cost of health costs and reduce the incidence of HAPI. Cheng et al.’s (2020) findings show that intensive care entities applying Rivera’s PIP buldles stand a chance to reduce HAPI cases to even zero. The scholars’ work informs the current work significantly. Cheng et al.’s study also serves as a motivation factor towards our institution’s intentions to study and utilize the intervention.
Significance of the Project
High healthcare costs present a significant problem for the United States (Padula & Delarmente, 2019). Prolonged hospital stays due to the development of pressure injuries in intensive care unit patients exponentially increase such costs. Treatment of superficial pressure ulcers costs about $500, while the price of more advanced HAPIs can rise to $70,000 (Padula & Delarmente, 2019). Every tenth patient in MICU in one urban New York hospital requires secondary interventions that increase the cost of primary care, thereby necessitating preventive measures that minimize these expenses (Rivera et al., 2020). In addition to economic benefit, patient outcomes and satisfaction will increase because the quality of life will be improved, allowing them to have shorter hospitalizations and return to their families early. Many clinical trials achieved a significant reduction in the HAPI incidence rate. A quasi-experimental clinical study by Anderson (2018) reached a seven-fold drop in the prevalence of pressure injuries. This project aims to utilize the quasi-experimental study design to determine how effective the selected scheme of the PIP bundle will be in the 13-bed MICU.
The problem of pressure injuries is widespread in the medical industry (WHO, 2008). Padula et al. (2019) argue that this health condition affects more than 2.5 million people. Padula and Pronovost (2018) also admit that HAPIs result in 60,000 deaths in the USA annually, and their costs are estimated at $9-$11 billion. Simultaneously, Li et al. (2020) argued that the HAPI prevalence is 12.8%, while the incidence rate is 5.4 for every 10,000 patient days (p. 2). The WHO (2008) states that HAPI prevalence is similar in different nations, including 10% in the USA, 11% in Germany, 12% in Sweden, and 13% in Israel (p. 45). These data indicate that a significant part of the US population is subject to this health condition. Simultaneously, the project site reports that it suffers from an 11% prevalence that refers to the incidence of 10 HAPIs per 100 patients. Thus, it is necessary to find a practical solution to minimize the incidence of HAPI and protect individual health.
The present study’s purpose is to help critical care units with the highest numbers of HAPIs incidences to manage the situation. The project particularly targets our thirteen-bed hospital located in New York. A major focus concerning the study is to provide a reliable evidence-based way of reducing HAPIs cases by proving or disapproving the effectiveness of Rivera’s PIP bundle. As such, the point that healthcare facilities, including ours, cannot bill the treatments related to HAPIs subjects hospitals to immeasurable cost burdens. The issue of wrong branding as a result of the high HAPIs cases in the entity is also targeted by the present study. The successful completion of the work thus stands to help our hospital, together with the other quality conscious healthcare facilities, to find solutions to one of the most probing issues in the care delivery line. The study’s timing appears appropriate based on the current situation where lots critical care facilities experience congestion due to the COVID-19 pandemic. Arguably, the study, together with several others that concern HAPIs and the possible interventions, are what the healthcare realm has been waiting to realize real transformation.
Rationale for Methodology
This quality improvement project used quantitative methodology to focus on measuring the impact of Rivera’s PIP bundle implementation on HAPI incidence rates. A quantitative methodology is useful for addressing clinical problems and answering clinical questions and relies on numerical data. Creswell and Creswell (2018) explain that the main benefit of the methodology is that it allows for an experiment to collect and analyze data and lead to conclusive results. Rutberg and Bouikidis (2018) stipulate that a quantitative method is appropriate when answering a clinical question that aims to achieve quality improvement.
This methodology was sufficient and effective for guiding how this quality improvement project was conducted. This project’s dependent variable is the incidence of HAPI, a quantity measured and reported in numeric values, thus proving suitable for a quantitative methodology. HAPI’s prevalence and mortality rates are also numerical values that are the focus of the project’s problem statement, thereby further justifying the use of a quantitative methodology. It is also suitable for addressing the project’s clinical question as it is suitable for making definite comparisons, such as the impact of Rivera’s PIP bundle compared to current practice. Therefore, the clinical question attempts to identify a measure of improvement, and the selected methodology frames the use of Rivera’s PIP bundle and statistical tests to find its answer and address the problem of HAPI among patients at the project site.
Nature of the Project Design
The quasi-experimental approach offers the best model to utilize in the present study. The approach follows the same steps like empirical design, but for the fact that it lacks the random assignment aspect. As such, the quasi experiment design answers questions by studying specific targeted population with the features or elements that the researcher is interested in (Harley, 2018). The quasi-experimental model stands out as one of the most reliable approaches for establishing causal effect(s) of an intervention on a particular target population. The assignment, however, occurs without the random assignment elements present in normal experimental designs (Harley, 2018).
A quasi-experimental approach is effective in handling a clinical problem and retorting a clinical inquiry. The point that the method utilizes numerical data makes the approach vital in identifying the specific incidence of the given phenomena. Quasi-experiments are like normal experimentation tactics, only that they are suitable for specific cases, like the one targeted by the present study (Harley, 2018). The methodology applies essential tests, like the t-test, which upsurges the dependability of the acquired upshots. Creswell and Creswell (2018) further note that one of the primary benefits of this statistical methodology is its ability to allow the steering of a trial to gather and evaluate the acquired data. Moreover, Creswell and Creswell (2018) specify that a quasi-experimental method is suitable when responding to a clinical problem to attain quality upgrading. As such, the incidence of HAPI cases constitute the dependent variable in this project, and form the quantity measured and stated in numeric figures. That way, the use of quasi-experimental design fully responds to the project’s clinical question, as well as addresses the problem statement effectively. Also, the present study’s clinical inquiry endeavors to isolate a degree of progress, while the designated approach runs arithmetical tests to deliver such an answer.
Definition of Terms
The following terms are operationally defined in lay words and in the context in which they appear in the paper.
Pressure Injury Prevention Bundle
This approach allows clinicians to have guidance for the assessment and monitoring of intensive care unit patients. This term refers to the plan of care that was developed to prevent the development of pressure injuries in patients at risk (Romanelli et al., 2018). The prevention bundle elements may vary between authors, but the overall goal of all methods is to prevent further complications of HAPI.
Pressure Ulcers (HAPIs)
This term denotes “areas of localized injury to the skin and underlying tissue, usually over a bony prominence, as a result of pressure, or pressure in combination with shear” (Li et al., 2020, p. 2).
Turning
The process is when individuals move or change their position while sitting or lying. Immobilized patients in MICU on vents with paralytics and sedation require help with turning.
Assumptions, Limitations, Delimitations
The following assumptions are present in this quality improvement project:
- It is assumed that the project participants do not create any treatment barriers and diligently follow the PIP bundle offered to them. This idea is necessary since it implies that changes in the HAPI incidence, if any, are directly related to the intervention, not external processes.
- Another assumption denotes that the project will identify the positive connection between providing a PIP bundle and the decreased HAPI incidence. This statement implies that the project aims at arriving at the conclusion that utilizing the PIP bundle is an effective pressure injury prevention intervention.
- One more assumption is that the healthcare facility correctly enters the data on patients’ pressure injuries in their EHRs. This condition is necessary because the project relies on EHRs to identify the HAPI incidence.
The following limitations are found in the project:
- Time constraints can be considered an essential limitation of the project. Since the project covers four weeks, it fails to assess the long-term effect of the proposed intervention.
- Another limitation is a small sample size because the project focuses on patients from a single medical facility in urban New York. It can be difficult to generalize the obtained results and determine whether the proposed intervention can be effective for the larger population.
- One more limitation is that the project depends on how accurately and diligently the facility approaches its reporting system. It relates to the fact that if the healthcare unit fails to mention in its EHRs that some patients experience pressure ulcers, the project’s results will suffer.
The following delimitations are found in the project:
- The project is delimited to a 13-bed critical care unit in urban New York. This delimitation is necessary because critical care patients are more subjected to pressure injuries due to poor tissue perfusion or hemodynamic instability.
- Another delimitation is that the project chooses a nursing theory by Jean Watson (2018) to ensure that the project has some theoretical support.
Summary
Chapter 1 presents all the basic elements concerning the present study. The section starts by offering a description of the major issue concerning HAPIs and the need to resolve them. The section also provides adequate background for the study and the clinical question to be answered, as well as the project’s endeavor to advance clinical knowledge. Other areas covered by the chapter include the rational for the study, nature of the project design, assumptions, and definition of terms.
Padula et al. (2019) explain that HAPIs are a significant problem in the healthcare industry, meaning that a practical intervention is necessary to address the issue. Chapter 1 has also formulated the problem statement, the purpose of the project, and the clinical question. Evidence from scholarly sources demonstrates that the project can advance scientific knowledge because the existing literature offers conflicting results of using the PIP bundle (Rivera et al., 2020). Thus, the project is significant since it aims at addressing this gap and providing multiple stakeholders, including patients, healthcare professionals, and the whole medical facilities, with essential benefits.
Chapter 1 also comments on the methodological aspect of the project. The intervention for reducing HAPI prevalence was presented in this chapter. Specifically, the background knowledge about the PIP bundle developed by Rivera et al. (2020) and some other variations of this approach are discussed in chapter 1. Creswell and Creswell (2018) justify using a quantitative approach, while Rutberg and Bouikidis (2018) explain that it is reasonable to use a quasi-experimental design. Then, the key terms are defined to ensure that anyone reading them accurately understand the concepts under discussion. The project assumptions, limitations, and delimitations have also been discussed in detail, while specific comments are offered on how to overcome these limitations in a future project. Chapter 2 presents an overview of the current literature on the PIP bundle and whether this intervention effectively prevents pressure injuries.
Literature Review
The present project endeavors to tackle the issue of HAPIs in the American healthcare facilities. HAPIs are a major cause of concern for everyone involved in care delivery, especially those serving in the critical care department. The U.S., for example, loses billions of dollars every year to HAPIs-related complications. About sixty thousand patients also lose their lives die to HAPIs-founded complication. The life of an individual is very expensive and precious. That is why the present project purposes to investigate the matter with HAPIs and the possible solution through the application of Rivera’s PIP bundle. The present literature review section thus addresses some of the critical scholarly information that addresses the same clinical problem, together with the targeted intervention.
The project aims to measure the effectiveness of Rivera’s PIP bundle in reducing health-acquired pressure injuries (HAPIs) among critical care patients. HAPIs are preventable conditions that often occur in the intensive care unit. They involve pressure injuries that cause localized skin and tissue damage due to intense and continuous pressure. The risk factors for developing HAPIs are immobility, altered mental status, and advanced age (Frank et al., 2017). This review aims to uncover the importance of implementing a PIP bundle in reducing the prevalence of pressure ulcers in critical care units.
This chapter first provides an overview of the literature selection process. Thus, it includes the search terms and databases used to obtain the literature along with the number of articles that were obtained and reviewed. The chapter then proceeds to describe literature concerning the project’s theoretical foundations. It explores Watson’s and Lewin’s theories concerning human caring and organizational change respectively. Then it proceeds to review literature concerning the project’s purpose, that is, implementing Rivera’s PIP bundle to reduce HAPIs in critical care settings. It reviews literature concerning the risk factors for HAPIs, various strategies for preventing HAPIs, and the usefulness of the PIP bundle as an intervention for HAPIs. The chapter then ends with a summary tying everything in the literature review to the project’s purpose.
A thorough literature review was performed to identify the existing information, beginning with professional databases to find credible and timely literature on the topic. The literature search was conducted using the following databases: EBSCO, Cumulative Index to Allied Health Literature (CINAHL), Ovid, PubMed, and Google Scholar. The following keywords and their various combinations were used to identify the required sources of information: pressure injuries, pressure injury prevention bundle, interventions related to pressure injuries, risk factors, and incidence related to pressure injuries. The search results are limited to the studies that were published not earlier than 2017 to ensure that the project deals with the most recent literature. The identified articles are included in the project based on their abstracts. The articles are included if they are available in full text and peer-reviewed. As a result, 90 studies were retrieved, while a set of 50 credible and reliable studies were selected for this literature review.
Hospital-acquired pressure injuries (HAPIs) cause several adverse effects to various parties. The problem, for instance, adversely affects patient care and further causes deleterious consequences for the healthcare system, especially, when it comes to health care costs and patient (Padula & Delarmente, 2019). It is vital to reduce incidences of HAPI, particularly in the ICU since it presents many problems. It has a major financial implication, with its cost extending beyond $2,000 per pressure injury (PI). The involved cost and associated human suffering explain the dire need to establish effective preventive strategies (Gaspar et al., 2019). High incidences can influence the affected organizations and lead to financial challenges. The National Quality Forum (NQF) considers most of the HAPIs preventable.
Theoretical Foundations
Jean Watson’s human caring theory identifies how to improve positive outcomes during human-to-human caring moments. The theory relies on practice, research, and theory-based education to ensure that any proposed intervention is suitable and can help patients achieve better health outcomes. They conducted a content analysis study to examine the opinions of interprofessional team members concerning a human caring model based on Watson’s theory. The study revealed the nursing theory enriches interhuman relations, establishes a holistic caring environment, and promotes patient care. Watson’s theory of caring helps create an excellent environment around the patients and staff to promote healing. Energetic authentic caring presence occurs when the nurse and patient come together to create a caring moment. Pressure injuries occur mostly in immobile and elderly patients and PIP bundle interventions, performed by the nurse or the healthcare team, such as repositioning an immobile patient can prevent pressure injuries, meet the basic needs of patient, and help sustain human dignity.
Jean Watson’s human caring philosophy covers the role of a nursing professional in the healing process. The model encourages nursing to engage their patients in positions that make self-healing possible. The nursing principle maintains that the nurse’s main role covers the aspects of health promotion, illness prevention, caring for the sick, and health restoration. Such implies the nurse’s central responsibility in promoting health and diseases’ treatment. As per Watson, caring is fundamental to nursing practice and encourages health better than a mere medical cure. Watson believes that that an all-inclusive attitude to health care is principal to the exercise of caring in the nursing profession.
Watson’s human caring theory informs the present project significantly. The work purposes to boost nurses’ knowledge concerning HAPIs management. The problem, HAPIs is a major concern in the present-day care provision realm. HAPIs make the process of healing difficult. The point that they account for about sixty thousand deaths a year also imply their adverse effects to the general nursing profession. As such, Watson maintains that the primary purpose of a nurse is to restore health and promote healing (Watson, 2018). Undertaking this study thus complies with Watson’s curative factor of applying scientific problem solving approaches for caring decision making.
The project focuses on a specific change theory. It refers to Kurt Lewin’s (1951) change management theory that is typically used for numerous quality improvement projects. This framework implies that patients change their behavior under the influence of driving or positive forces that affect individuals from outside (Lewin, 1951). This information suggests that it is necessary to provide patients with external support to ensure that they can overcome some challenges. The Lewin change model implies that the project will rely on specific steps to measure the variables. First, it is necessary to improve patients’ knowledge about the problem and its possible solutions, Lewin’s stage of unfreezing (Burnes, 2020). The next step involves implementing the change, which involves establishing the solutions within the organization, Lewin’s stage of changing. Finally, after being evaluated as effective, the change is established as the industry standard concerning solutions to the problem; Lewin’s stage of refreezing. Lewin’s change theory is important to the project as it delineates processes for instigating Rivera’s PIP bundle in acute care settings where they have not been implemented before. As a result, the change will encounter obstacles and resistance that necessitate the change model for effective transition.
Review of the Literature
The literature review assessed evidence-based practices to explain existing challenges in prevention of HAP. The literature identified gaps in the existing research and suggested areas for further study. The literature review built an argument on the development of the clinical question while explaining the current models, topics, and theories. It will enable the reader to understand the importance and relevance of the project. The literature review process revealed evidence organized into the following themes: Hospital acquired pressure injuries, Risk factors and Pressure injury prevention bundle.
Hospital-Acquired Pressure Injury
Hospital-acquired pressure injury (HAPI) affects patient care; it is associated with deleterious consequences for the healthcare system and patient (Padula & Delarmente, 2019). It is vital to reduce incidences of HAPI, particularly in the ICU since it presents many problems. It has a major financial implication, with its cost extending beyond $2,000 per pressure injury (PI). The involved cost and associated human suffering explaining the dire need to establish effective preventive strategies (Gaspar et al., 2019). Moreover, the scope of the problem is high and involves multiple levels. Rivera et al. (2020) revealed that at least one million people develop PI annually in the U.S. The study also indicated that 2.3 million patients in acute care facilities develop the condition where more than 60,000 lose their life due to related complications (Gaspar et al., 2019). High incidences can influence the affected organizations and lead to financial challenges. The National Quality Forum (NQF) considers most of the HAPIs preventable. Additionally, CMS does not provide reimbursements for HAPIs thereby eliminating payments to hospitals for their care (Padula et al., 2020).
Incidence Rates
Chaboyer et al. (2018) conducted a systematic review and meta-analysis that examined the problem of pressure ulcers that emerge as a result of clinical treatment in terms of scale and scope. The conclusions are made based on the in-depth analysis of twenty-two studies that were reviewed and synthesized in alignment with the research questions. Chaboyer et al. (2018) report the cumulative incidence of HAPIs to be within the range of 10-26%. These numbers indicate that the matter at hand represents an issue of a serious magnitude. As for the location of the HAPIs, the systematic review indicates that most of them emerge on the patient’s sacrum, followed by the buttocks, heel, hips, ears, and shoulders (Chaboyer et al., 2018). Accordingly, pressure ulcers affect a considerable number of patients, causing moderate-to-severe discomfort in the fallout of prolonged care.
Li et al. (2020) explored the issue from a global perspective, utilizing the international experience to address their clinical question. More specifically, they aim to quantify the prevalence and incidence of pressure injuries and the hospital-acquired pressure injuries rate in hospitalized adult patients (Li et al., 2020, para. 2). In order to address the research purpose, the authors rely on the formats of systematic review and meta-analysis. The research sample comprises cross-sectional, observational, and longitudinal studies that report HAPIs among hospitalized adults. Based on the examination of forty-two relevant studies and a total sample of 2,579,049 patients, Li et al. (2020) report an incidence rate of 5.4 per 1,000 patient days. Most of the HAPI cases represent stages I and II of the condition (71.5% in total). From a geographical perspective, the analysis revealed a considerable level of heterogeneity, implying certain territorial correlations that are to be explored in subsequent examinations. This study highlights that the prevalence of HAPIs is a global healthcare concern, but its exact magnitude may vary across different settings.
According to Anderson (2018), HAPIs have high significance for patients in critical care. He defines them as pressure injuries that cause localized skin and tissue damage due to intense and continuous pressure. He also reports on their incidence rates in intensive care units varying from 14% to 42%. During a quasi-experimental clinical study for addressing HAPIs, Anderson (2018) reached a seven-fold drop in the prevalence of pressure injuries. As a result, he recommended that hospitals place readily available resources for nurses to utilize when monitoring and intervening on the pressure injuries.
HAPI Impact on the Healthcare System
The elevated incidence rates of HAPIs are concerning for all parties involved in the delivery of medical services. In this regard, healthcare organizations equally sustain considerable damage, primarily in the financial domain. Padula and Delarmente (2019) extend this discussion even further, attempting to evaluate the national burden of hospital-acquired pressure injuries in the United States. To address the research question, the authors of the research rely on a Markov simulation. Through this method, they estimate the costs of staged HAPI’s that emerge during hospitalization from a medical organization’s point of view. As per the simulation’s results, the annual HAPI costs for the U.S. healthcare system exceed $26.8 billion, which is a colossal amount. Moreover, the distribution of the costs is not proportionate, as nearly 60% of the amount is a condition by the less frequent Stage III and Stage IV cases of pressure injuries. Therefore, the prevalence of HAPI’s undermines the financial aspect of the system, impeding the quality development of hospital units. In this context, significant progress can be made through the prevention of advanced-stage pressure injuries, alleviating the economic burden on organizations.
The immense economic impact of hospital-acquired pressure ulcers remains a matter of increased concern for the system’s management. Lim and Ang (2017) investigate this aspect of the problem within their research. The clinical report is based on the experience of a tertiary hospital in Singapore, thus contributing to the international dimension of the discussion. The clinical questions are presented from the managerial perspective, aiming at reducing the operational costs of healthcare organizations. The authors rely on the famous assumption, stating that the prevention of a problem is widely recognized as more effective than its treatment. In this regard, healthcare organizations are encouraged to pursue new avenues of reducing the incidence rates of HAPI’s like a phenomenon. These ideas align with the ongoing trends within the academic community, as researchers investigate the root causes of pressure injuries in order to develop stronger interventions. The examination by Lim and Ang (2017) reveals that HAPIs are a major stressor for hospitals, depleting their finite resources through prolonged stays, patient dissatisfaction, and corresponding expenses. Therefore, the impact of HAPIs on healthcare organizations is concerning, thus justifying the need for effective interventions.
The problem of HAPIs is global in nature, making it necessary to synthesize and implement the world’s best practices into intervention projects. Han et al. (2019) follow the data obtained through practical observations and analyses in a South Korean hospital with increased HAPI incidence rates. The clinical question was whether these conditions affected the key parameters of a healthcare organization’s performance. More specifically, the authors of the study associate HAPI’s with a strong negative impact on the patient’s health. The sample of 1,000 patients was compared with a 4,000-person control group. The results indicate that advanced HAPIs are associated with increased mortality rates, putting additional pressure on patients and medical units. In addition, the average duration of stay for the patients who develop this condition is longer, leading to higher healthcare costs and financial burdens. Finally, the emergence of HAPIs is a serious predictor of readmission, which, in turn, equally undermines the performance of a medical organization. Therefore, all parties involved in the clinical procedure will benefit from effective interventions aimed at the prevention of hospital-acquired pressure injuries.
The information presented in this section confirms the multi-faceted adverse impact of HAPIs on the functioning of medical organizations. In today’s environment, hospital units work with limited resources. In fact, the efficient distribution of these resources is an essential enabler of better healthcare outcomes that improve the patients’ well-being, promote public health, and sustain the system’s development. The presented findings indicate a major degree of negative influence by the HAPIs, undermining the system’s capacity to fulfill its obligations for the community. Increased healthcare costs are an overarching theme of these discussions, meaning that HAPIs become a serious financial burden for organizations. However, in addition to this, the repercussions of unaddressed HAPIs extend beyond these ideas, contributing to the increase of mortality and readmission rates in hospitals. When all these factors act combined, the prevalence of pressure injuries translates into major healthcare issues that encompass the primary aspects of the system, in general.
Patients with Specific Health Conditions
As can be inferred from the prior discussion, a number of underlying conditions can aggravate the development of HAPIs. Typically, this health issue is the most acute for individuals who spend much time in prone or sitting positions. However, other factors can facilitate the emergence of pressure injuries, prompting scholars to seek specialized methods for such particular cases. Thus, it is reasonable to identify research pieces that would make it clear whether PIP bundle is helpful for people with particular health conditions.
In addition, cardiovascular conditions may entail serious complications in stressful environments. Chitambira and Evans (2018) assessed the effect of repositioning for stroke patients with pusher syndrome and using a quality improvement initiative with 140 adults. The researchers draw attention to 2-hourly repositioning and placing of pillows. This article supports the claim that repositioning becomes more effective when it is used together with an additional intervention. Since the study focuses on a short intervention period, the authors highlight the necessity to organize further research on this topic. A retrospective descriptive article by Cox, Roche, and Murphy (2018) argues that immobility and septic shock are among the most common pressure ulcer risk factors. Pittman, Beeson, Dillon, Yang, and Cuddigan (2019) offer another descriptive retrospective study highlighting that HAPIs can be preventable and unpreventable. The unavoidable HAPI occurs among patients with bowel management devices (Pittman et al., 2019).
As pressure injuries affect the skin tissue, corresponding health issues may also aggravate the development of this condition. Gray and Giuliano (2018) reveal that there is a robust correlation between pressure injuries and incontinence-associated dermatitis (IAD). A descriptive and correlational analysis of 5,342 adults demonstrates that an increased HAPU prevalence is found when it comes to focusing on IAD patients. The authors highlight that traditional prevention measures, are not sufficient to protect the population from the given health condition. Thus, another argument in favor of a combined approach is made. Razmus and Bergquist-Beringer (2017) state that pediatric patients are subject to the issue, while Hultin, Karlsson, Öhrvall, and Gunningberg (2019), Latimer et al. (2019), and others explain that older patients are at risk.
However, the range of underlying conditions is not limited to oncology, skin diseases, or cardiovascular issues. Mussa et al. (2018) focus on pressure injuries among patients with an endotracheal tube (ETT). A retrospective, pre-post intervention study indicates that a more frequent repositioning leads to some improvements, but they are not statistically significant. The authors prove it by analyzing data of 61 members from the pre-intervention group and 81 individuals from the post-intervention group. This finding demonstrates that it is not possible to rely on only one preventive intervention repositioning and turning exclusively to protect patients with ETTs from HAPUs.
The damage to a patient’s spine is a serious matter per se, limiting the mobility of a person. Eren, DeLuca, and Kirshblum (2020) consider what results preventive interventions offer to patients with spinal cord injury. The authors do not implement any interventions but interview such individuals regarding whether they rely on the intervention. The findings demonstrate that almost half of the 86 respondents fail to turn regularly, irrespective of the fact that they are aware of this action. That is why it is not surprising that patients with spinal cord injury are subject to HAPUs.
Risk Factors
Risk factors contributing to the development of HAPI ‘s in the clinical setting revolve around identifying and categorizing the primary predictors of pressure injuries that occur during a patient’s prolonged stay at a facility (Dreyfus et al., 2017). HAPIs are a major societal burden that can be addressed effectively and prevented if major underlying causes are correctly determined. Some of the risk factors identified by Kayser et al. (2019) during a longitudinal study include older age, male gender, unable to self-ambulate, all types of incontinence, additional linen layers, longer durations of stay, and being in an intensive care unit (p. 46).
Malnutrition
According to Greenwood and McGinnis (2016), malnutrition is one of the root causes for increased incidence rates of HAPIs in acute care. However, analysis suggests that patient pressure injuries rarely appear from a single cause; instead, they arise from a combination of factors. The authors of the study refer to HAPI emergence as a sequence of events that leads to adverse consequences in terms of patients’ well-being. Greenwood and McGinnis (2016) place malnutrition among the most important causes of HAPIs. They used data analysis methods to process the findings obtained by the root cause analysis process implemented in the U.K. since 2010. The practical purpose of such research was for identifying the key themes and learning points that can help develop meaningful solutions to the clinical issue in question. The research sample comprised thirty-two HAPI RCA’s that provided insight into the root causes of the pressure ulcers.
Predictors and determinants of HAPIs form an area of intense interest for researchers across the globe. Kayser et al. (2019) conduct their study to explore the differences between risk factors associated with a superficial and severe case of HAPIs. They analyzed 216,626 complete patient datasets from acute care hospitals in the United States. Having generated the annual linear trendlines, Kayser et al. (2019) performed two logistic regressions to examine the risk factors. The accumulated risk factor list comprised increased age, male gender, unable to self-ambulate, all types of incontinence, additional linen layers, longer durations of stay, and being in an intensive care unit (Kayser et al., 2019, p. 46). In addition, a U-shaped relationship between HAPI risks and body mass index was observed. In this context, both extremely low and high BMIs were associated with increased pressure injury risks. The study showed nutrition is a significant risk factor for HAPIs with deficiencies and obesity in nutrition causing increased risk for HAPIs.
Immobility
Kennerly and Yap (2018) conducted a review that included adverse effects of immobility. They investigated the impact of manual turning for improving the health outcomes of patients in critical care. They demonstrated that manual turning helps patients avoid adverse musculoskeletal and cardiovascular effects of immobility. They attributed the effect of immobility to gravitational equilibrium which makes it more difficult to ascribe to positional changes. As patients grow resistant to position changes, they become immobile. The effect of immobility is reduction in plasma volume, change in bone mass, and change in muscle mass. These effects expand the adverse effects of medical devices on the patients’ skin leading to pressure ulcers. Additionally, they make patients more prone post-operative fever and pneumonia that increase their ICU days and degrade their health outcomes.
A retrospective descriptive article by Cox et al. (2018) argues that immobility and septic shock are among the most common pressure ulcer risk factors. Patients in ICU are usually inactive and exposed to the risk of developing HAPIs. Cox et al. (2018) conducted a study to analyze and describe the risk factors for pressure ulcers in MICUs. The study used a sample of 57 patients all of whom experienced pressure ulcers while they were highly immobile in acute care. The injuries generally developed after 7 days and were mostly deep tissue pressure injuries around the sacrum. The study demonstrated immobility to be a significant risk factor for pressure injury development among acute care patients.
Damage to a patient’s spine may limit their mobility. Eren et al. (2020) examined preventive interventions offered to patients with spinal cord injury with a descriptive, non-experimental study. The study did not implement any interventions; instead, the study team interviewed individuals with spine injuries regarding whether they reposition themselves. The findings revealed that almost half of the 86 respondents failed to turn regularly, irrespective of the fact that they are aware of this action; thus, it is not surprising that patients with spinal cord injury are subject to HAPUs.
Poor Circulation
Risk factors for HAPI development include hemodynamic instability and vasopressors (Cox et al., 2018). Cox et al. (2018) conducted a descriptive analysis study to determine the risk factors for pressure injuries among patients in critical care. Among the sample of 57 patients who participated in the study, 50 identified with sedation as a risk factor for developing pressure injuries, 53 identified with head-of-bed elevation angle being greater than 30, and 37 identified with vasopressor use. These risk factors are highly associated with hemodynamic instability as they alter blood pressure by constricting blood vessels (vasopressors), decreasing the patient’s pulse rate (sedation), and introducing body positions that restrict optimal blood flow (head-of-bed elevation greater than 30) (Cox et al., 2018). Therefore, the risk factors show poor circulation to be a significant causative agent for pressure injuries among patients in critical care units.
Cardiovascular conditions may entail serious complications in stressful environments. Chitambira and Evans (2018) assessed the effect of repositioning for stroke patients with pusher syndrome and using a quality improvement initiative with 140 adults. The researchers draw attention to 2-hourly repositioning and placing of pillows. This article supports the claim that repositioning becomes more effective when it is used together with an additional intervention. Since the study focuses on a short intervention period, the authors highlight the necessity to organize further research on this topic.
Dreyfus et al. (2017) explored the risk factors contributing to the development of HAPIs in the clinical setting. They utilized U.S.-based data to address their clinical question. It revolved around identifying and categorizing the primary predictors of pressure injuries that occur during a patient’s prolonged stay at a facility. The authors refer to HAPI s as a major societal burden that can be addressed effectively and prevented if major underlying causes are correctly determined. They investigated 47,365 HAPI cases among 16,967,687 patients with a cumulative incidence of 0.28% including patients with health problems commonly associated with or resulting in poor circulation: history of diabetic foot ulcers and prior incidence of pressure. As per the findings, the prior incidence of pressure injuries is the most important predictor of future cases, along with a history of diabetic foot ulcers. Thus, they showed that hypertension and diabetes are high risk factors for HAPIs as they dysregulate blood flow in the patients.
Individuals with altered skin status are considered to have a high risk of new ulcer development. Shi et al. (2018) argued that there is insufficient evidence to support the potentially prognostic relationship. The study attempted to review the existing evidence systematically to understand the relationship between the development of pressure ulcer risks and skin status. A comprehensive electronic database search was performed in February 2017 to explore longitudinal studies that used skin status to support the prediction of pressure ulcers. It considered multivariable analysis studies where two reviewers independently selected studies. Data was collected on skin status, participants, as well as the characteristics of studies. This helped gather data on multivariable analyses of pressure-ulcer and the associated skin status. The article covered 41 studies involving 162,299 participants, out of which 7382 had new ulcers. It concluded that there exists low-certainty evidence that individuals suffering from non-blanchable erythema are at an increased risk of developing new pressure ulcers compared to those free from the condition. Further, low certainty evidence was noted for the prognostic effects of different skin descriptors, particularly the pressure ulcer history. These findings imply that there is a need for the adoption of improved preventive measures and skin assessment for patients with non-blanchable erythema.
The above subthemes provide detailed descriptions of the risk factors for HAPIs according to the literature. They present the major risk factors as poor circulation, immobility, and malnutrition. Understanding risk factors is essential to effective prevention of illnesses. Therefore, the next section proceeds to some ways pressure injuries can be mitigated
Pressure Injury Prevention
Preventive strategies can help decrease the incidence and impact of HAPI on the healthcare system and patients. Preventing pressure ulcers (PU) protects patient safety and comfort, and is a more cost-effective approach than treating HAPI when they develop. The three prevention components in this theme are positioning, skin assessment, medical device-related interventions, and PIP Bundles. The content presented includes the Rivera PIP bundle selected for implementation as the project intervention to address the problem and clinical question (Rivera et al., 2020).
Positioning
Turning patients is one of the interventions that is widely applied to relieve pressure from prone areas. Kennerly and Yap (2018) conducted a review that included adverse effects of immobility. They investigated the impact of manual turning for improving the health outcomes of patients in critical care. They demonstrated that manual turning helps patients avoid adverse musculoskeletal and cardiovascular effects of immobility. They attributed the effect of immobility to gravitational equilibrium which makes it more difficult to ascribe to positional changes. As patients grow resistant to position changes, they become immobile. The effect of immobility is reduction in plasma volume, change in bone mass, and change in muscle mass. These effects expand the adverse effects of medical devices on the patients’ skin leading to pressure ulcers. Additionally, they make patients more prone post-operative fever and pneumonia that increase their ICU days and degrade their health outcomes. As a result, proper positioning instigated by manual turning led to better health outcomes and reduced ICU days.
Aljezawi and Tubaishat (2018) attempt to determine whether turning and repositioning, offloading and application of preventive dressings are effective for cancer patients. A multicenter, cross-sectional prevalence study of 110 patients used a quantitative methodology to analyze the impact of 2-hourly repositioning on protecting such individuals from the health issue under analysis. The scholars conclude that irrespective of short frequency, this intervention does not guarantee that pressure injuries will not develop in some patients, such as those with cancer.
A cross-sectional prevalence study by Courvoisier et al. (2018) focuses on 2,671 patients to identify and compare the effectiveness of various intervals. These intervals are considered independent variables, while HAPU incidence represents a dependent one. Thus, the scholars have determined that 2- and 3-hourly intervals are more effective than 4-hourly ones. It demonstrates that a higher intervention frequency leads to improved health outcomes for patients suffering from HAPUs.
Skin Assessment
Comprehensive skin assessment involves the examination of the entire skin of an individual for abnormalities. It entails touching and looking at the skin while paying attention to the bony prominences. The examination is meant to detect present pressure ulcers and offer assistance in the risk stratification. This is done because patients with underlying pressure ulcers are at increased risk of developing more (Rivera et al., 2020). The assessment determines the presence of skin-related factors linked to the development of pressure ulcers, including moisture-associated skin damage (MASD) or excessively dry skin. It also enables the identification of other skin conditions and provides data required for the calculation of prevalence and incidences.
The type of intervention in patients varies depending on the Braden score. According to the bundle designed by Rivera et al. (2020), patients with a Braden score above 19 should receive the standard intervention. In contrast, patients with points equal to or below 18 will get high-risk intervention (Rivera et al., 2020). Implementation of this bundle resulted in a significant reduction in the occurrence of pressure ulcers (Rivera et al., 2020). Specifically, the index of healthcare-associated pressure injuries, which is the proportion of patients with pressure ulcers to the days spent in the hospital, dropped from 3.4 to 0.48 over the ten months (Rivera et al., 2020). The authors developed the bundling scheme with time intervals, but they do not discuss the intervention components in detail.
Effective skin assessment can support early detection and influence the implementation of an appropriate intervention. Bates-Jensen Wound Assessment Tool (BWAT) can be applied in clinical practice to assess wound healing. Bates‐Jensen et al. (2019) evaluated the application of the BWAT to assess home residents with a pressure injury. The study reported pressure injury characteristics including natural history, anatomic, and stage location among racially and ethnically diverse residents. The prospective 16 weeks study covered 142 participants with 305 pressure injuries representing a prevalence of 34%. Subepidermal moisture and visual assessment were attained from heel, ischial, buttock, and sacrum ulcers every week. The study revealed that BWAT is an effective assessment tool because it offers objective and reliable data to support the detection of the progress of pressure injury healing.
Early detection and identification of pressure damage risk need to be prioritized. Kim et al. (2018) evaluated the association between the application of sub epidermal moisture measurement and visual assessment of early pressure ulceration. The study employed a descriptive prospective observational design where data was obtained from at-risk patients in Ireland within an acute care facility. Obtained data included researcher-led sub-epidermal moisture measurements and the patient’s skin condition. With a sample of 47 patients who had a mean age of 74.7 years, 19 patients suffered stage 1 pressure ulcers and elevated sub-epidermal moisture (SEM) levels. Results showed 83% specificity, where the majority of false positives lacked adequate follow-up time. The study noted a medium correlation between SEM findings and nurses’ visual skin assessment.
The SEM measurement tool required 1.5 days to detect damage, while nurses took an average of 5.5 days. This implies that SEM measurement can detect early damage about days ahead of the nurse assessment. Early detection of the pressure ulcers damage is beneficial because it develops within the deeper tissues. This can enable the adoption of effective prevention strategies before worsening the condition. Moreover, early detection can limit the associated mortality and morbidity, reduce the length of hospital stay and improve patients’ experience.
Yafi et al. (2017) presented preliminary case studies showing the feasibility of spatial frequency domain imaging (SFDI) to promote assessing skin status in pre-existing wounds and high-risk populations. The technology involves the use of wide-field non-contact optical imaging with structured light to examining tissue constituents and optical properties. A near-infrared SFDI system was used to image patients at an increased risk for pressure ulcers. The study concluded that SFDI is a feasible optical technology that can be applied to assess blood volume status and tissue oxygen saturation quantitatively. It can offer an effective approach for pressure ulcer healing, risk stratification, and staging.
Medical Device-Related Interventions
Pressure-reducing devices have proven effective in the prevention of HAPI in critical care settings. Static devices are appropriate when supporting patients who can independently change positions. An air-fluidized or low-air-loss bed is effective for patients with non-healing or multiple large ulcers. Accumulated risk factors for the HAPI include the inability to self-ambulate, male gender, old age, extended hospital stay, additional linen layers, hospitalized in an intensive care unit, and incontinence. Extremely low and high BMIs are linked to a high risk of developing pressure injuries (Rivera et al., 2020). Prior cases of hospital-acquired pressure injuries increase the chances of developing new instances. Spending much time in a sitting or prone setting is another factor that increases the risk. Therefore, pressure-reducing devices prevent HAPI by mitigating the effects of poor circulation, immobility, and malnutrition that lead to pressure injuries.
Prevention devices, such as pressure-relieving mattresses, special cushions, and heel-elevating boots may benefit patients in acute care, as well as nursing home residents. These devices operate by lessening pressure created on the skin and enhancing the patient’s comfort. Some devices alternate periodically to move pressure points to lower extensive pressure on one body part through a mechanical system that deflates or inflates air cells in the mattress to attain the required comfort. Moreover, special pads can be applied to soften the surface or lower pressure and avoid the development of ulcers. Kamikawa et al. (2018) explained that a special pressure-relieving mattress could be used to hinder the development of ulcers among patients with a high risk. Long-term facilities and hospitals should consider installing these mattresses when handling immobile, comatose as well as elderly residents and patients.
The application of preventive dressing on intact skin can significantly reduce shear forces and tension between the support surfaces and the skin. This helps lower shear forces within the underlying soft tissues and the skin. Hahnel et al. (2020) investigated whether the preventive dressing is effective when handling patients in the high-risk intensive care units. The study evaluated the effectiveness of preventive multilayered soft silicone foam dressing when applied with standard prevention approaches. The objective was to determine whether it could lower deep tissue injury (DTI) and cumulative PU incidence for categories II, III, and IV. Eligible patients were aged at least 18 years who were expected to remain in the ICU for more than 3 days. The risk assessment was based on the care dependency and mobility of patients. The study concluded that the use of preventive dressing and standard care could help prevent PUs among high-risk patients in the ICU. Unlike other interventions such as repositioning, special support surfaces, mobilization, and floating heels, the application of preventive dressing presents an easy-to-apply approach.
The use of prophylactic dressings can offer an effective strategy to support the prevention of pressure ulcers by enhancing the distribution of external pressure. They prevent friction and shear damage by hindering pressure in high-risk patients. Cornish (2017) confirmed that the application of a prophylactic dressing presents many benefits when considered in the holistic pressure ulcer prevention strategy. The dressing is examined from time to time without causing trauma or pain to patients making it an effective option. However, the article recommends nurses consider promoting hygiene and good nursing care to achieve the best outcome. The additional components of temperature, humidity, friction, and shear should motivate clinicians to establish a holistic approach to support high-risk patients. Prophylactic dressings can retain sufficient moisture to promote elasticity in the skin while reducing skin stripping, excoriation, and maceration. It also can retain the heat necessary for the healing process.
Rivera Pressure Injury Prevention Bundle
Pressure ulcer prevention is a significantly compounded process. There are various items that ought to be deliberated and accomplished in the approach. Inaugurating superlative practices is also a perplexing task that necessitates the implementation of a ‘care bundle’ to aid the integration of such best observations. The bundle approach involves the advancement of the best practices and systematic application of the same. Definite care practices are valuable in assisting the achievement of the anticipated results (Rivera et al., 2020). The bundle needs to include numerous critical mechanisms, including all-inclusive skin assessment, identical risk assessment, care planning, wound care nurse consultation, as well as medical device-related mediations.
Bundle’s evidence-based approach demonstrated its effectiveness in various quality-improvement clinical trials. Standardized intervention methods are essential assets in preventing pressure injuries. For example, several evidence-based interventions, known as a bundle, are more efficient when introduced in combination (Frank et al., 2017). The classical prevention bundle consists of five items: skin assessment, surface support, mobility and repositioning, incontinence, and nutrition (Romanelli et al., 2018). Frank et al. (2017) presented the results from 33 pediatric hospitals that implemented the prevention bundle and found a twofold decrease in the incidence of stage 3 and 4 pressure injuries (Frank et al., 2017). The authors concluded that introducing the bundle approach can ensure the early detection of pressure injuries and reduce the prevalence of late-stage ulcers.
Critical components of the Rivera PIP bundle include comprehensive skin assessment, care planning, standardized risk assessment, wound care nurse consultation, and medical device-related interventions (Rivera et al., 2020). Standard risk interventions should consider different aspects of care and improve the existing practices. It can be tailored to a specific setting and supported with additional steps to ensure successful implementation. Key practices need to be achieved regularly to overcome the challenge of improving care. It ensures that every component of the bundle is performed consistently through the creation of a clinical pathway.
Similar to the Rivera PIP bundle, Gupta et al., (2020) used multidisciplinary clinical and risk assessment teams to test various changes as well as implementing an effective program including skin inspection, the surface, nutrition, incontinence, and keep moving bundle. Strategies to engage staff included PI incidence calendars, turning clocks, and signs as reminders in the unit. The study revealed an 83.5% reduction in HAPI incidences and a 9.7% drop in prevalence. It was concluded that the PIP bundle is an effective tool for the reduction of pressure injuries.
Other quality-improvement clinical studies also evaluated the effectiveness of the bundle approach. A systematic review by Lin et al. (2020) demonstrated a significant reduction in the prevalence of pressure ulcers in US hospitals after introducing the bundle approach of various components. The components of Rivera bundle include: comprehensive skin assessment, care planning, standardized risk assessment, wound care nurse consultation, and medical device-related interventions. However, most of the evaluated trials did not report the significance of their studies (Lin et al., 2020); further, the authors admit that there was no link between the number of components in bundles and the outcome. The retrospective study by Singh et al. (2018) examined data from 99 pediatric hospitals that implemented prevention bundle methods. The authors showed a mean drop of pressure injury incidence by 57% across hospitals (Singh et al., 2018). Still, the scholars are not sure about the reliability of the information because they could not control the data collection process.
Summary
In summary, hospital-acquired pressure injuries are an ongoing problem across the world (WHO, 2008), the nation, and in local healthcare facilities. Although there is growing evidence supporting the prevention of pressure injury, there exists a gap in the implementation of effective preventative strategies. Thus, HAPI continue to occur, causing detrimental impacts on hospitals and long-term care facilities, and on the lives of patients and their loved ones.
The use of the PIP bundle can support the standardization of PIP strategies, protect at-risk patients, and influence a reduction in pressure ulcers (Rivera et al., 2020). An evidence-based PIP bundle initiative needs support from the leadership and involved staff. The impact on the patient outcome negatively hinders nurse satisfaction. They are associated with the increased cost of medication, prolonged hospital stays, poor patient experience, and a high rate of mortality. Risk factors for HAPIs development include sedation, immobility, hemodynamic instability, and vasopressors.
The reduction of HAPIs and the implementation of PIP bundle necessitate a comprehensive approach while establishing a sense of ownership among nurses, involvement, engagement, and support of every stakeholder. The PIP bundle initiative is enhanced when health care workers show commitment to the provision of quality care to patients (Wei & Watson, 2019). Reducing HAPIs as well as maintaining the momentum is a major challenge affecting many critical care units. Implementing the integrated approach is an expensive process making it difficult for many hospitals to adopt despite its benefits. Moreover, there exists a gap in the literature, and further research is needed to improve the level of bundle evidence for the PIP implementation.
Chapter 3 presents the project methodology, beginning with the problem, purpose and clinical question. The selected methodology and design include the population and sample for the project, sources of data and the process to collect it, as well as aspects of data analysis including statistical testing. Chapter 3 also present factors involved in the integrity of the project: validity, reliability, potential bias, ethical considerations, and limitations.
Methodology
The present research work addresses a fundamental healthcare issue that affects population’s health unfavorably. The project thus endeavors to determine whether the application of Rivera’s PIP bundle can help reduce HAPI frequency in critical care units. As such, the research work’s aim is to identify whether the application and implementation of the specific PIP bundle helps in managing HAPIs more effectively relative to the present practice among many healthcare facilities. Consequently, the project proceeds through the application of appropriate methods to find answers to the inquiry.
This chapter’s aim is to elucidate the particulars of conducting the project. The purpose is thus to to state the exact details of the utilized approach. In this chapter, the clinical question, problem, design, suitable methodology, sample, and population are reflected. The chapter also remarks on the appliances and sources applied to acquire the project’s data. The different facets’ validity, as well as reliability, are also described. Moreover, the project’s data collection and analysis techniques are also clarified in detail. The section further provides satisfactory narrative concerning the possible bias and vindication efforts. As such, all this evidence is necessary to validate the manner in which the project was conducted to make replication and reviewing possible.
Statement of the Problem
It was not known if or to what degree the implementation of Rivera’s PIP bundle would impact HAPIs’ frequency when compared to current practices among the critical care patient in a 13-bed unit in urban New York. HAPIs present a significant problem to health care as they affect more than 2.5 million individuals in the United States and cause up to 60,000 deaths (Padula et al., 2019). Moreover, there is insufficient literature addressing the problem concerning its prevention and treatment. Therefore, the present DPI project aims to address its prevention and treatment through Rivera’s PIP bundle in a critical care unit that reports HAPI incidence rate of 14%, which is higher than the national average that stands at about nine percent.
Clinical Question
The present project acquires its direction from the question: To what degree does the implementation of PIP bundle impact the HAPI incidence when compared to current practice among hospitalized critical care patients in a 13-bed unit in urban New York over four weeks? The clinical query is essential to direct the focus of the research work. The question further discloses the rudimentary information on how the research work is going to take place, comprising the projected intervention, and selected scenery. A rephrased version of the research question is as below:
Q1: Is usage of Rivera’s PIP bundle more effective when compared to current practice?
The clinical question presents the correspondence of the project’s variables. PIP bundle is the independent variable in the study. Nurses must apply PIP bundle for every patient in critical care unit during the study. The HAPI incidence further forms the dependent variable for the study. The factor is measured both pre- and post-mediation to determine whether the employment of the independent variable effects quality improvement in the HAPIs situation.
A between-group approach is further utilized to answer the clinical question. The tactic implies that contributors in the mediation and assessment groups are dissimilar. The intermediation (after) group primarily includes persons who received the offered mediation. As such, the research participants, including wound care nurses and head nurses of the utilize unit collect cumulative data on the sample size to recognize the number of pressure injuries occurring, which introduces the need to adopt and utilize the patients’ electronic health records (EHRs).
Project Methodology
The project utilized a quantitative methodology, which is appropriate as it relies on numerical data and is necessary for identifying the incidence of the pressure injuries. Creswell and Creswell (2018) states that the main benefit of the quantitative approach is that it provides statistical means for collecting and analyzing data. Bell et al. (2018) also admit that it applies different statistical tests, including t-test, which increase the reliability of the obtained results. Rutberg and Bouikidis (2018) stipulate that a quantitative method is appropriate for answering a clinical question that aims to achieve quality improvement. Since the project’s clinical question focuses on HAPI incidence, which represents a quality improvement project with numerical significance, the quantitative methodology is the most optimal option.
While a quantitative method focuses on identifying numerical representations of an issue, a qualitative approach is typically used for exploring and establishing new knowledge regarding a phenomenon (Creswell & Creswell, 2018). As a result, the qualitative approach is unsuitable for the project, which has already determined HAPIs to be a significant health care problem and seeks to measure whether Rivera’s PIP bundle will decrease its incidence rates. Furthermore, qualitative methodologies are typically more resource and time consuming. The quantitative methodology is the best approach since it focuses on the credible measurement of numerical data and manages to answer the clinical question.
The present project focuses on reducing incidence rates of HAPIs in a critical care facility. As a result, a quantitative methodology is most appropriate for the study as incidence rates are numerical data. Therefore, the quantitative methodology best aligns with the numerical data collection and analysis techniques utilized when comparing incidence rates before and after implementation of the project’s intervention. Additionally, a quantitative methodology increases the simplicity of the project’s implementation, which then does not focus on complicated textual data analysis. Simple statistical analysis techniques, such as t-test, provide sufficient means for evaluating the project’s outcomes.
Project Design
This quality improvement project utilizes the quasi-experimental design is it carries the advantages of an experimental design, involving measurement of causality between an intervention and an outcome without applying randomization that is time- and resource-intensive. Thus, the quasi-experimental approach is time- and resource-efficient for identifying correlation between the project’s dependent and independent variables (Rutberg & Bouikidis, 2018). Rutberg and Bouikidis (2018) reiterate that the design allows assessment of an intervention’s effectiveness for experimental and control groups. Siedlecki (2020) also admits that case studies, descriptive, and correlational designs are not appropriate for causality measurement since they are less practical and involve less measurements. Thus, the quasi-experimental design is ideally aligned with the quantitative methodology.
The present project focuses on applying Rivera’s PIP bundle intervention and identifying whether it leads to improved outcomes (reduced HAPI incidence). The independent variable that is the intervention is the use of PIP bundle. HAPI incidences are measured before the intervention’s implementation for the comparison chart review group and after its implementation for the intervention group. The PIP bundle components used in this project are based on standard- and high-risk interventions. According to the bundle designed by Rivera et al. (2020), patients with a Braden score above 19 should receive the standard intervention. In contrast, patients with points equal to or below 18 will get high-risk intervention (Rivera et al., 2020). These interventions include skin assessment, medical device-related interventions, wound care nurse consult, application of preventive dressings, turning, offloading and nutrition consult. Head nurse and wound care nurses were responsible for ensuring that the nurses followed the intervention. The dependent variable was the HAPI incidence rate that was measured by focusing on the number of patients who developed pressure injuries during their hospital stay. The data for the dependent variable was collected by analyzing electronic health records after the end of the intervention process. Wound care nurses accessed the records to stipulate how many pressure ulcers developed.
First step of the project was to collect the pre-intervention data. The nursing staff was provided with education on the PIP bundle. Staff education of all elements of PIP bundle was very critical to preventing HAPIs. The education was continuous to provide necessary support to the staff. Head Nurse and Wound Care Nurses provided the necessary training in all shifts. Nurses then implemented the PIP interventions for patients according to their assessed risk: standard-risk versus high-risk. The following data were collected for the intervention population four weeks after the education had been completed and the PIP bundle interventions had begun: age, gender, and number of new HAPIs.
Population and Sample Selection
The present study focuses on the population comprising of all individuals that attend the selected research facility for treatment. The term population, as applied in here, mainly refers to adults of diverse ages, nationalities, and sexes. The chosen organization had three hundred and seventy-one staffed beds during the time of study. This number thus forms the basis from which the project sample is established. Consequently, the project also involves the unit staff members in its population.
The research work’s sample further comprises of hospitalized critical care patients admitted to the facility’ adult intensive care section. The choice is informed by the fact that such patients exhibit increased HAPI risks. The aged populating in the unit has unbalanced vital signs and spends much time lying or sitting. The sample is based on the 13-bed unit of the selected institution. The research utilizes a non-probability expediency sampling technique. Such implies that participants participating in the study do so because of their availability in the investigation center. The approach is beneficial in that it guarantees sample diversity (Jager et al., 2017). The point that no stringent exclusion standards are applied in the project makes the benefits real. The research work utilizes a before and after-design that necessitate the availability of two sets of patients. The before (assessment) group includes patients recorded to visit the unit four weeks before the study. The after (mediation) set is what receives the PIP bundle.
All the accessible patients admitted to the unit are involved in the mediation. The intervention procedure suggests that members of the after receives the PIP bundle through the intervention of the head. Consequently, all the partakers’ data will form the basis of the analysis stage to ascertain the HAPIs’ incidence. The project’s sample size thus equals the total of people involved in the instruments. Being admitted to critical care unit and ailing from urban New York form the main criteria for the sample. Working with the wound nurses and the application of coding system further promotes confidentiality during the project.
Instrumentation or Sources of Data
The project use electronic health records (HER) to gather data. Wound care nurses at the target unit will assemble data from EHR. The nurses will then provide the HAPI incidence statistics to the researcher without the name of the patients, as well as the medical record number. The information will help in assessing the HAPI incidence at the facility at the presence of the researcher. The intervention’s measurement application is crucial because of the evidence-based practice aspect.
Electronic Health Records (EHRs)
EHRs will be accessed from the unit’s electronic data storage devices. The facets contains information concerning the individual history of pressure ulcer. The EHRs include all the details directly related to patients’ individual health. Epic system is that EHR tool utilized by the selected health facility. Nurses exhibit the responsibility of completing the documentation in Epic system at the facility.
Moreover, wound care nurses acquire such data from the system for reporting. Epic offer a significantly dependable platform that is utilized for documentation of new hospital acquired pressure injuries during the study. The investigators ensure that the patient information is protected by not copying or distributing the information. The investigator will get data from the wound care team. The researcher will also get a Health Insurance Portability and Accountability Act (HIPAA) waiver of authorization to ensure access to the patients’ medical data from the facility.
Validity
Validity measures an instrument’s capability for producing true results. Rivera’s PIP bundle’s validity is evident in its ability to reduce incidence rates of HAPIs when implemented among adults in a critical care facility. Rivera et al. (2020) developed the PIP bundle which assigns intervention to patients in acute care who have developed HAPIs depending on the severity of tissue damage. They tested the bundle’s effectiveness in an 11-bed critical care unit in one of the hospitals in New York City (Rivera et al., 2020). As such, Hernandez-Boussard, Monda, Crespo, and Riskin (2019) state that the validity of electronic health records is higher than 95%, meaning that the project deals with decent external validity since it ensures that the instrument focuses on the issue.
Reliability
Reliability measures an instrument’s capability for presenting consistent results when implemented under similar circumstances. Rivera et al. (2020) demonstrated their PIP bundle’s reliability by testing its results for the same sample population over time. Interventions present in the bundle vary depending on the Braden score. Patients with a Braden score above 19 receive the standard intervention while patients with points equal to or below 18 get high-risk intervention (Rivera et al., 2020). Implementation of this bundle resulted in a significant reduction in the occurrence of pressure ulcers (Rivera et al., 2020). Specifically, the index of healthcare-associated pressure injuries, which is the proportion of patients with pressure ulcers to the days spent in the hospital, dropped from 3.4 to 0.48 over the period.
Data Collection Procedures
The investigator contacted the selected critical care facility in urban New York and obtained facility permission for conducting the project within its setting and to receive the data from wound care nurse. The project also required approval from the Institutional review board at the facility and Grand Canyon University for permission for this project. Data collection did not begin until the investigator received all required approvals. Pre-intervention data for the project consisted of HAPIs incidence rates within the selected critical care unit during the four weeks immediately prior to the implementation of Rivera’s PIP bundle. The data was available in the hospital’s EHR and the hospital’s wound care nurse provided the investigator deidentified data on the patients who developed HAPIs in that designated timeframe.
Before the intervention’s implementation, nurses received training on how to use Rivera’s PIP bundle to assess pressure injuries among critical care patients in their unit and to implement necessary prevention and treatment strategies. Their education included on elements of PIP bundle and proper EHR documentation. The data included the patients’ demographic data and whether they contracted HAPIs during their stays. The nurses also received education on appropriate privacy and security measures because they were in contact with the patient data. Numbers were assigned to the participants as the coding system to ensure confidentiality. If a participant had experienced a pressure ulcer, 1 was placed while 0 denoted that no HAPI had occurred. As part of the security measures, the notes were not made available as automated reports and were not uploaded to web clouds to avoid a digital information leak. Instead, they were stored in a locked cabinet within the critical care unit that was only accessible by the chief investigator. The data files are kept for three years post-intervention as reference points after which they are to be physically destroyed to prevent any misuse of this information.
The project’s main focus was the post-intervention data that was useful for measuring the intervention’s effectiveness in reducing HAPI incidence (the project’s dependent variable). It was the HAPI surveillance details that the wound care nurses and head nurses gathered after the intervention was implemented. They included the number of patients who contracted HAPIs during their hospital stay after the attending nurses had implemented Rivera’s PIP bundle for HAPI prevention and treatment. The data also included the patients’ demographic information and their medical status information. The nurses recorded the data during the four weeks after the start of the PIP bundle implementation in paper charts which they stored in a locked cabinet within the critical care unit. After the four weeks elapsed, they provided the deidentified data to the EHR team for digital storage and analysis. The project’s focus was the aggregate and not the individual patients’ data. The following section comments on how the obtained results can be analyzed to arrive at appropriate conclusions.
Data Analysis Procedures
Upon completion of the project, the researcher identified data from the IT team and loaded the coded data into excel to prepare the data for analysis using SPSS, version Logo icon, v27. The question guiding this project is: To what degree does the implementation of PIP bundle impact the HAPI incidence when compared to current practice among hospitalized critical care patients in a 13-bed unit in urban New York over four weeks? The independent variable, PIP bundle, is the project’s intervention and is absent in the comparison groups. The HAPI incidence is the project’s dependent variable, and it is necessary to compare this value for two independent groups. For that purpose, the independent t-test is suitable since this inferential statistical test measures the difference between the means of two groups. This parametric test is appropriate to the project since the latter follows a before and after design, meaning that two groups should reveal the effect of the intervention.
The first step of running the t-test is to prepare the raw data. The coding system, where 1 refers to a HAPI and 0 denotes its absence, produces categorical data. It is necessary to create two tables with numbers 1-64, and each line should contain either 1 or 0, depending on whether the participant has experienced a pressure ulcer. Since the t-test focuses on the means, the second step is to calculate this measure for the two samples. Once these values are obtained, it is possible to conduct the third step of running the t-test to identify whether the difference between the measures is statistically significant. The specific level of the statistical significance (p<.05) is chosen to ensure that the obtained results are statistically significant and minimize the effect of chance. This requirement is also necessary because it justifies that the findings are scientifically valuable. Finally, all the materials acquired during the study were stored for six months; when the period was over, their hard copies were physically destroyed by burning.
Potential Bias and Mitigation
Scientific studies are subject to numerous biases that adversely affect the quality of work, and quantitative articles often face threats that undermine their internal validity. Internal validity refers to the degree to which the results are accurate and that permits causal inferences to be made regarding the association between the independent and dependent variable (Flannelly et al., 2018). There can be intentional and unintentional bias, and it is the investigator’s moral responsibility to address all the possible issues that can invalidate the project’s results. Consequently, the given section comments on what biases may be in the project and how they can be mitigated.
Sampling bias can occur because the project deals with non-probability convenience sampling, especially when some outcomes are favored over others (Fowler & Lapp, 2019). Convenience sampling can produce inferences that are not as trustworthy as if a random sampling technique is used. However, this bias is mitigated because the sample selection procedure did not have many inclusion and exclusion criteria. Patients are included in the project because they are currently available to the investigator. Consequently, this approach is also advantageous because it ensures that samples are sufficiently diverse (Jager et al., 2017). Therefore, potential bias from convenience sampling was mitigated.
Bias may adversely affect the data collection process (Fowler & Lapp, 2019). The selection bias implies that the project’s results can be impacted because some patient groups are underrepresented while others are over-represented. It can occur because people can be more or less likely to participate in the project. The project utilizes a convenience sampling technique that focuses on a single criterion to overcome this potential issue. If patients are available to the investigator, they are offered to participate in the project.
Manipulation or misinterpretation of the data may cause or contribute to data analysis bias (Fowler & Lapp, 2019). The investigator ensured that the data analysis procedure was transparent, described in detail, and strictly followed. The project collected, analyzed, and reported aggregate data, and appropriate statistical test was used to determine statistical significance of the intervention in relation to the project’s dependent variable.
The project focuses on ensuring that no bias affects the data interpretation step. Since a between-group design is employed, the t-test for independent groups is used because this parametric statistical test measures the difference between two independent groups (Creswell & Creswell, 2018). Furthermore, the project is not only focused on a single side of the problem. For example, even if the proposed intervention does not show statistically significant improvement in reducing the HAPI’s incidence, the project demonstrates whether the process results in other clinically significant improvements.
Ethical Considerations
A significant ethical issue relates to the fact that the project deals with patients’ EHRs. The challenge is that these records contain protected health information according to the HIPAA; it is necessary to obtain permission from the chosen facility. In this case, the project demonstrates that all the ethical issues are addressed. Simultaneously, the investigator ensures that confidentiality, anonymity, and privacy are present. For that purpose, the coding system is applied to use numerals instead of participants’ personal details. This requirement is necessary to protect personal data from disclosure.
The IRB approval is necessary since it should claim that it is a quality improvement project rather than research. This approval demonstrates that the investigator can proceed to data collection. The IRB approval letter is included in Appendix A to indicate that the project meets the requirement. Since the project is deemed a quality improvement one that is generally applied to all patients, there is no necessity to obtain informed consent from the participants. Furthermore, it is reasonable to admit that informed consent is also not required because the project deals with aggregate, not individual data. The site authorization letter is found in Appendix B, and it demonstrates that the chosen facility permits the investigator to conduct the project in the selected setting. Conflict of interest is absent because the investigator is not biased in completing the project in a particular way to achieve specific results. Full transparency is present in the project to prove the statement above.
The project adheres to the principles of the Belmont Report,as stipulated by the US Department of Health and Human Services (1979):respect, justice, and beneficence (Adashi, Walters & Menikoff, 2018). The principle of respect is ensured because no individuals are coerced to be involved in the project against their will. Thus, respect is found in the projects’ sample selection procedure. The principle of justice is present in the sample recruiting process since no bias is applied to representatives of a certain age, gender, or ethnic group. Simultaneously, the principle of beneficence is found in the project design and the theoretical framework. It refers to the fact that human subjects’ well-being is addressed because members of the two groups receive adequate care. In addition to that, the principle of beneficence is present in the project because no individuals involved in the scientific process are subjected to harm.
Hard copies of the coded materials will be stored in a locked cabinet in a safe place. The project does not involve the creation of digital copies of these data. The project’s results will be published as a requirement of the investigator’s Doctor of Nursing Practice. Finally, the materials will be stored for three months; when this period is over, their hard copies will be physically destroyed using a paper shredding machine.
Limitations
The project is subject to a few limitations. The research work, for example, refers to a small sample size since it focuses on few individuals from a single 13-bed critical care unit. Even though such a sample size is unavoidable when dealing with the narrow critical care setting, it is difficult to generalize the obtained results. Thus, the findings cannot be applied to representatives of other population groups. However, this limitation should not affect the findings negatively because the power analysis revealed that the sample size was sufficient. Furthermore, the focus on patients of a single facility allows for assessing the intervention’s effectiveness in the given context. This information can help identify an efficient way to prevent pressure ulcers among critical care patients.
Second, the project’s results are limited by its design and short timeframe. The quasi-experimental project lacks randomization and does not focus on long-term effects. This QI project uses convenience sampling, not random sampling, so concessions are implied and accepted with this type of sampling. This fact also demonstrates that it is impossible to generalize the findings. However, this weakness is delimited because the statistical test is used to assess specific outcomes in the short run. Additionally, this limitation is not negative since it brings some advantages. For example, the absence of randomization denotes that the project does not require many financial resources and much time. Focusing on a limited time frame can also be advantageous since it assesses the short-term effectiveness of the chosen intervention to reduce the incidence of pressure injuries.
Third, a significant limitation exists because the project’s results depend on how accurately the EHRs are created. This weakness is unavoidable in the given design because healthcare professionals are responsible for making these records. In particular, nationally certified wound care nurses and head nurses of the unit will collect the aggregate data on HAPI incidence and insert it in the EHRs. However, this limitation should not generate many negative results because the project assumes that the healthcare professionals will perform these functions diligently and attentively.
The project has delimitations set out by the investigator. First, the project facility is chosen explicitly because its nursing staff welcomes the use of evidence-based practice. The facility has an existing culture that promotes the implementation of quality improvement initiatives; the selected site has a rich history of dealing with multiple health issues. Thus, the decision to focus on the 13-bed unit is a significant delimitation of the given project. This information justifies the assumption that the facility staff will actively and diligently participate in the project.
Second, the focus on the specific population is also a delimitation because it ensures that the project will produce specialized findings. Luo, et al., (2019) explain that people of 60 years old and higher are more subjected to pressure ulcers. This information denotes that it will be possible to use the project findings as a guide to prevent HAPIs among hospitalized patients and improve the population’s health. Third, the use of a nursing theory by Jean Watson (2018) is another delimitation. This step ensures that the project has solid theoretical support as well as a caring perspective of patients.
Summary
HAPIs present a significant problem to health care as they affect more than 2.5 million individuals in the United States and cause up to 60,000 deaths (Padula et al., 2019). Therefore, the present DPI project aims to address its prevention and treatment. The project’s clinical question was: To what degree does the implementation of Rivera’s PIP bundle impact the HAPI incidence when compared to current practice among hospitalized critical care patients in a 13-bed unit in urban New York over four weeks?
The project utilizes a quantitative methodology, which is appropriate as it relies on numerical data and is necessary for identifying the incidence of the pressure injuries. It utilizes the quasi-experimental design is it carries the advantages of an experimental design, involving measurement of causality between an intervention and an outcome without applying randomization that is time- and resource-intensive. The project focuses on applying Rivera’s PIP bundle intervention and identifying whether it leads to improved outcomes (reduced HAPI incidence). The independent variable that is the intervention is the use of PIP bundle. HAPI incidences are measured before the intervention’s implementation for the comparison chart review group and after its implementation for the intervention group. The population consisted of adult patients who presented to the selected urban New York hospital and were admitted to critical care for various ailments and medical conditions. Patients admitted to critical care formed the subset of the population that comprised the project sample as they were at increased risk for developing HAPIs.
The project’s dependent variable is HAPI incidence rate. It represents the main data collected before and after the implementation of Rivera’s PIP bundle by the wound care nurses at the NYC critical care unit. The investigator collected the project’s deidentified data from the wound care nurse. This data was retrieved from EHR by the wound care nurse, which represents the project’s primary source of data. Rivera’s PIP bundle’s validity is evident in its ability to reduce incidence rates of HAPIs when implemented among adults in a critical care facility. Rivera et al. (2020) tested the bundle’s effectiveness in an 11-bed critical care unit in one of the hospitals in New York City and demonstrated a seven-fold decrease in HAPI incidence. They also demonstrated their PIP bundle’s reliability by testing its results for the same sample population over time. Implementation of the bundle resulted in a drop of the index of HAPIs, which is the proportion of patients with pressure ulcers to the days spent in the hospital, from 3.4 to 0.48 over ten months.
Data collection did not begin until the investigator received all required approvals from the selected critical care facility in urban New York and the Institutional review board at Grand Canyon University. Pre-intervention data for the project consisted of HAPIs incidence rates within the selected critical care unit during the four weeks immediately prior to the implementation of Rivera’s PIP bundle. Before the intervention’s implementation, the investigator educated the nurses on how to use Rivera’s PIP bundle to assess pressure injuries among critical care patients in their unit and to implement necessary prevention and treatment strategies. As part of the security measures, the notes were stored in a locked cabinet within the critical care unit that was only accessible by the chief investigator. The project’s main focus was the post-intervention data that was useful for measuring the intervention’s effectiveness in reducing HAPI incidence (the project’s dependent variable). The primary investigator collected the deidentified data from the wound care nurse and loaded the coded data into excel sheets for analysis. The primary investigator utilized the Excel software and SPSS software to perform various statistical tests, including t-tests, which compared the post-intervention data to the pre-intervention data to measure the intervention’s effectiveness.
The project is subject to numerous biases that adversely affect the quality of work and undermine its internal validity. Sampling bias could have occurred because the project dealt with non-probability convenience sampling where some outcomes could have been favored over others. However, the bias was mitigated because the sample selection procedure did not have many inclusion and exclusion criteria. The project was also liable to selection bias due to some patient groups being underrepresented while others are over-represented. It utilized a convenience sampling technique that focused on a single criterion to overcome this potential issue. Finally, manipulation or misinterpretation of the data may have contributed to data analysis bias but the investigator ensured that the data analysis procedure was transparent, described in detail, and strictly followed. The project adhered to the principles of the Belmont Report: respect, justice, and beneficence. It adhered to the principle of justice by mitigating bias in the participant selection phase, the principle of beneficence by not subjecting the participants to harm, and respect by considering the inputs of participants and beneficiaries. However, it was limited by a small sample size, short timeframe and accuracy during EHR creation.
The analysis and results of the project comprise the remainder of the project report. Chapters 4 and 5 follow the implementation of the PIP bundle intervention. Data description, variable data analysis procedures and results appear in Chapter 4. The project summary, findings, and conclusions, as well as theoretical, practical, and future implications and recommendations for future progress and practice are in Chapter 5.
Data Analysis and Results
The purpose of this quantitative, quasi-experimental project was to determine if or what degree implementation of Rivera’s Pressure Injury Prevention (PIP) bundle would impact HAPIs prevalence rate as compared to current practice among critical care patients in the Urban New York acute care hospital over four weeks. The project considers the development of pressure ulcers among patients in the critical care units. It explains how the problem affects the quality of health care among hospitalized patients.
It was not known if or to what degree the implementation of Rivera’s PIP bundle would impact HAPIs prevalence rate when compared to current practice among patients in critical care unit. Specifically, with an average age of 64, this unit reports the prevalence of pressure ulcers of 14%. Furthermore, 55% of all pressure injuries in the hospital are found in this unit. Older patients often experience mobility problems, and their skins are damaged through dehydration. Certain medical conditions among the population can hinder the effective flow of blood, influence movement problems, and make skin more fragile.
The project utilized numerical data to determine the prevalence of pressure ulcers and enhance collection and analyzes of data. The reliability of the results will be improved by the use of statistical test. A quantitative approach was adopted because it is marked with increased clinical relevance and facilitates answering of the clinical question. The study involves a quantitative and quasi-experimental design to determine whether the implementation of a PIP bundle can reduce the prevalence of HAPIs among patients in critical care units. Jean Watson’s human caring nursing theory is effective in examining the effectiveness of the bundle. The theoretical framework of Kurt Lewin’s (1951) change management theory supported the analysis of forces and subsequent balancing of the change plan. The theory offered an effective framework for the preventive bundle. Lewin’s Change Theory entailed a three-step change model, and it is effective in supporting the implementation of interventions to enhance the achievement of desirable changes in nursing. The purpose of the project is to measure the HAPI incidence rate during the patients’ hospital stay upon the implementation of the PIP bundle. For this purpose, the wound care team accessed EHR to identify whether a patient experiences a pressure ulcer.
Clinical question attempts to evaluate the degree of the PIP bundle implementations impacting the HAPI incidences among patients in critical care units within four weeks. This compares the effectiveness of the PIP bundle with that of the current practice. The clinical question determined whether implementation of PIP bundle has a greater impact of reducing HAPI incidences than current practice in a 13-bed unit in urban New York over four weeks. The clinical question helps suggests the intervention approach as well as the study settings.
The PIP bundle offered a beneficial audit tool to support the provision of valuable information concerning adherence and knowledge gaps. It focused on improving documentation in the EHR and reduction of pressure injuries among patients in the critical care units (Hahnel et al., 2020). The WOC nurses were encouraged to influence and reinforce the use of the PIP bundle during wound consults and rounds since it was not part of the EMR. The training was provided on specific areas to improve their ability to treat patients and implement the bundle effectively. WOC nurses also reviewed and instructed documentation during consultations and daily briefs. Reinforcement was ensured by every health provider during PIP rounds and daily briefs.
Audit results offered beneficial information concerning adherence to the bundle and existing gaps in documentation. The litigious environment linked to pressure ulcers shows that gaps in knowledge are of critical importance. The project team had to ensure that nurses are well educated on key issues such as documentation and the treatment process. All professionals, including the nurse manager, resource nurses, and physicians, encouraged the staff to ensure adherence (Hahnel et al., 2020). The bundle was implemented in the critical care unit, and measures were established to ensure its sustainability. Stakeholders were encouraged to remain vigilant and determined in the prevention of HAPI.
Descriptive Data
Table 1present the demographic data of the patients included in the analysis of this project. The sample population (N=XX)for both the, comparative group n=XX, XX%)and post-implementation group (n=XX, XX%) included males, (n=40, 62.5%) and females (n=24, 37.5) females. Their ages ranged from 28 to 86 and the median age was 66.
Table 1. Results For Pre- And Post-Intervention Data
Table 2 presents the description of primary diagnoses recorded for both the comparartive group and post-intervention groups included medical cardiac problems such as congestive failure or myocardial infarction (n=20), endocrine (n=6) and renal problems(n=10), gastrointestinal (n=16) and pulmonary ailments (n=12). Data on HAPI incidence among the sample population was collected before and after receiving Rivera’s PIP bundle treatment to hinder the development of pressure ulcers.
Table 2. Primary Diagnoses Among Sample Population
Data Analysis Procedures
Data was extracted from the unit’s electronic record by the wound care nurses and later was analyzed using t-test statistical methods. Wound care nurses provided de-identified data to the primary investigator. The investigator obtained the required data before and after the implementation of the PIP bundle.
The comparison data collection engaged nurses with the standard practices for pressure injury prevention. Education and training were done before the bundle implementation. The appropriate nurse-to-patient ratio was maintained to ensure the satisfaction of all bundle requirements. The unit nurses were held responsible for implementing all interventions based upon the Rivera’s PIP bundle. Data collection was done by analyzing the implementation compliance differences before and after the Rivera’s PIP bundle intervention. The prevalence of pressure ulcers was measured before and after the bundle intervention.
The raw data consisted of demographic information and HAPI incidence among the sample population. The Excel and SPSS software were utilized to perform various statistical tests, including t-tests that compared the intervention data to the comparison data to measure the intervention’s effectiveness. The clinical questions sought to identify to what degree does the implementation of Rivera’s PIP bundle impact the HAPI incidence compared to current practice among critical care patients in a 13-bed unit in urban New York over four weeks? The data collected was for patients in critical care suffering from myocardial infarction, endocrine problems, renal problems, gastrintestinal ailments and pulmonary ailments. The data was organized stating the existing ailment and how they responded to the intervention. Data was organized such that there statistics for presence of HAPIs without intervention using PIP Riveras bundle treatment and the presence of HAPIs after the use of the Riveras PIP bundle.
The utilization of the various statistical tools in the present study was informed by several rationals. The t-test, for example, is a highly essential statistical data analysis tool that is highly applicable in experimental designs. The tool works well under at least two statistical conditions. One of such situations is an experimental state in which some subjects receive some kind of treatment, while a control condition does not. As such, t-test is excellent in situations exhibiting comparison in performance in the two conditions. Occasionally, differences between study conditions are very clear-cut, indicating that an experimental treatment has made a clear difference to subjects’ behaviour. However, the difference between research conditions is not so obvious. That is why the t-test is highly essential. In such circumstances, t-test can helps to determine whether the variance between the research conditions is genuine or whether it is owed merely to chance fluxes from one phase of testing to another (Abbott, 2017). The t-test enables researchers to decide if the mean of one condition is actually dissimilar from the average of another condition. The point that the present study features such elements thus ascertains the appropriateness of t-test’ utilization during the project.
The t-test is one of the most commonly used statistical methods in medical research papers. The statistical approach (t-test) can be divided into at least two sub-paradigms. One of such is the one-sample t-test, while the other type is the two-sample t-test. The tool is inappropriate to compare the means among more than three groups (Abbott, 2017). Concretely, one-sample t-test is utilized to compare a single group’s mean value to a specific (single) number, for example, a known population mean (Abbott, 2017). The two-sample t-test, on the other hand, is a kind of inferential statistic applied to determine whether there is a noteworthy dissimilarity between the averages of two groups (Abbott, 2017). Notwithstanding, the two-sample t-test exists in two forms, the independent sample t-test (group t-test) and paired t-test. The former, independent sample t-test, is performed when the samples characteristically consist of independent study populations. The paired (correlated) sample t-test is further utilized when an observation in one group is linked with a related observation in another group (Abbott, 2017). The samples in a paired sample t-test classically comprise of matched pairs of similar units. The paired samples t-test tool is also highly recommended when there are cases of repeated measures. Consequently, the statistical tool to apply in the present project was the independent sample t-test. The point that the research work utilizes averages obtained from two independent groups forms adequate ground for the choice.
The t-test belongs to the group of parametric assessment tools. Such (parametric) tests exhibit significant assumptions, including normality, variance homogeneity, and independence. The assumptions must be satisfied to ensure the correct use of t-test, according to (Abbott, 2017). Additionally, the theoretical supposition of t-test maintains that the test can only be useful to the quantitative data of single factor design. It is, therefore, inappropriate to perform t-test for multifactor design, such as conditions involving several independent factors or variables, like different types drug dosage and gender, for example. As such, the kind of data handled in the present project complies with the basic assumptions of the t-test. Such an aspect thus makes the utilization of the t-test in the present project valid and appropriate.
The utilization of SPSS, for Windows 14.0., in this project is also appropriate. SPSS is the abbreviation for ‘Statistical Package for the Social Sciences’ (Abbott, 2017). The statistical tool is utilized by numerous kinds of researchers to handle complex statistical data analysis processes. The SPSS software package was fashioned for the organization and statistical analysis of social science data. SPSS was formerly launched in 1968 by the SPSS Inc., before its acquisition by IBM in 2009, leading to the name IBM SPSS statistical tool. As such, SPSS finds much of its utilization in the marketing and health sectors. Government entities, survey companies, education investigators, data miners, and marketing groups, among other groups find SPSS high useful for processing and analyzing research data, including research information gathered through online survey platforms (Abbott, 2017). The visualization designer is one of the core functions of SPSS. The program allows researchers to use their data to generate a wide range of visuals, like radial boxplots and density charts, from the survey data with comfort. Abbott (2017) notes that SPSS software combines together a number of programs in a single package. The fundermental application of the software is to analyze scientific data connected with the social sciences. Consequently, the point that the present project covers social science subject ascertains the effectiveness of using SPSS for data analysis.
The SPSS analytical tool helps researchers to generate a meaning from the acquired statistical information. Marketing scholars, for example, manage to understand the demand for a product in the market, and thus devise an appropriate change of strategy to fit the anticipated targets. Principally, SPSS first stores and organizes the provided research data before compiling the same (data) set to produce apposite output. Abbott (2017) cheers SPSS because of its special design that makes possible for the program to handle an enormous set of variable data formats.
Microsoft excel is the other essential statistical program utilized in the present project. Excel is undoubtedly the most frequently applied spreadsheet program for personal computers in the research world. The program comes installed in many newly purchased computers, hence highly available. Excel exhibits several attractive features, such as the ease of application, availability, and affordability (Abbott, 2017). The program manages several statistical evaluations and calculations with ease, courtesy of the installed collection of statistical functions and a Data Analysis ToolPak (Abbott, 2017). Consequently, Microsoft Excel offers convenient solution to researchers seeking to undertake simple statistical analysis or in case where other expensive statistical programs are hard to find. Abbott (2017) argues that excel offers significantly rare convenience for data entry and speedily manipulation of rows and columns prior to statistical analysis. However, the scholars insist on the need to utilize the likes of SPSS, SAS, or Systa, when handling more critical research analysis processes. As such, the present project utilized excel for such reasons, which offered convenience and promoted data analysis operations during the study.
Results
To what degree does the implementation of Rivera’s PIP bundle impact the HAPI incidence compared to current practice among critical care patients in a 13-bed unit in urban New York over four weeks? The statistical analysis equation for the t-test tool is t = observed difference between sample means minus difference between population means under the null hypothesis, divided by the estimate of the standard error of the difference between the two sample means. The equation is represented as t = (Ẍ1-Ẍ2)/ √(S2(1/n1+1/n2)). In this formula, t is the t-value, Ẍ1 and Ẍ2 are the means of the two groups being compared, s2 is the pooled standard error of the two groups, and n1 and n2 are the number of observations in each of the groups.
Table 3 below provides the results of the project’s t-test. Results of the study answered the clinical question by confirming that the implementation of the PIP bundle reduced the incidences of pressure ulcers. The comparative group data collection engaged nurses with the standard practices for pressure injury prevention. Education and training were done before the bundle implementation. The appropriate nurse-to-patient ratio was maintained to ensure the satisfaction of all bundle requirements. The unit nurses were held responsible for implementing all interventions based upon the PIP bundle. Data collection was done by analyzing the implementation compliance differences before and after the PIP bundle intervention. The prevalence of pressure ulcers was measured before and after the bundle intervention.
Table 3. t-Test for Pressure Ulcers’ Incidence Mean Scores by Group
The above output table provides the project’s t value, the degree of freedom, and the acquired p value. From the output table, it is clear that the difference in means for the sample data is 5.084 (t(63) = 5.084), while the confidence interval shows that the true difference in means is between 4.836 and 7.333. As such, ninety-five percent of the time, the true difference in means will be different from 0. The project’s p-value of 0.025 (p =.021), which is much smaller than 0.05, so the study rejects the null hypothesis of no difference and maintains, with a high degree of confidence, that the true difference in means is not equal to zero. Consequently, the t-test proves that the application of Rivera’s PIP buddle causes real positive effect to the HAPIs’ incidence in the healthcare system. Moreover, Table 4, below, provides information concerning the real changes in pressure ulcers’ incidences courtesy of the PIP buddle intervention. The table shows that applying the initiative leads to about thirty percent reduction in incidences, which is a significant improvement.
Table 4. Reduced Incidences of Pressure Ulcers
Based on the acquired results, the project also revealed that pre-intervention training improved nurse’s confidence and familiarity, and subsequent compliance. Feedback and review of clinical manifestations facilitated the successful implementation of the PIP bundle and supported the development of professional behavior (Gaspar et al., 2019). High compliance was ensured by the development of an audit behavior checklist. The approach is an effective strategy to satisfy the individual needs of patients.
An audit tool was utilized to facilitate compliance, and it contained a series of yes or no questions. Table 3 below illustrates the checklist to analyze the achieved level of adherence. Table 3 answers whether the patient had this assignment or not. The PIP bundle was recorded upon satisfaction of the audit tool contents. In case a single requirement was not meet, results were recorded as unimplemented. The creation of awareness and training of nurses influenced a high level of adherence to the bundle implementation resulting in the achievement of a desirable outcome.
Summary
Results from the project show that HAPIs can be managed through the application of PIP bundle approach. The project’s t-test results provide a highly dependable information regarding the effectiveness of the intervention. The data shows that PIP bundle is effective in the reduction of PIs among adult patients in critical care settings. Implementation of the bundle significantly reduced incidences and promoted patients safety (Rivera et al., 2020). The project used an intervention group who received care with the PIP bundle. The pre-intervention group did not receive the PIP bundle and their retrospective data was collected prior to the implementation of the intervention with the intervention group. The provided data and subsequent analysis were relevant to the clinical question since they explained the process and impact of the PIP bundle implementation.
The data also helped determine beneficial preliminary measures that need to be considered to influence the success of the integrated approach. These include training and educating nurses to build their confidence and familiarity. Another important factor is the engagement of all stakeholders and encouraging everyone to play a role in ensuring that success is realized (Rivera et al., 2020). The development of an effective culture can support the implementation of the bundle because since it can support coordination, hard work, and desire to achieve the best outcome. The outcome of the study encouraged the implementation of the PIP bundle in a diverse setting to lower the chances of developing PIPs among patients with an extended hospital stay.
Chapter five will summarize the project and explain the importance of the topic, its contribution to the body of knowledge while providing recommendations. It will highlight important points in the study to help the audience attain a brief understanding of the entire project. It will offer a comprehensive recap of the applied procedures, obtained results while explaining its importance in the nursing field. By offering a summary of the results, it will provide details of the achieved outcome.
Summary, Conclusions, and Recommendations
The clinical question guiding the project was: To what degree does the implementation of Rivera’s PIP bundle impact the HAPI incidence compared to current practice among critical care patients in a 13-bed unit in urban New York over four weeks? The question sought to identify whether using Rivera’s PIP bundle would be sufficient to reduce the HAPI incidence within the critical care unit. The project utilized a quasi-experimental approach to answer the clinical question. The wound, ostomy, and continence nurses (WOC nurses) collaborated with stakeholders to organize and develop the implementation plan. The bundle implementation over four weeks influenced a massive reduction from the pre-intervention to the post-intervention.
The following chapter provides a summary of the entire project. It covers the project’s purpose, design, setting, data collection and analysis techniques, and the results. It then presents a summary of the discussion regarding the results and the consequent conclusion. It discusses implications of the study’s design, results, and conclusions. These include the theoretical, practical, and future implications of the quality improvement project. The chapter then ends with recommendations for future projects and practice.
Summary of the Project
The project’s clinical question was: To what degree does the implementation of Rivera’s PIP bundle impact the HAPI incidence compared to current practice among critical care patients in a 13-bed unit in urban New York over four weeks? It aims to identify patients at an increased risk for the development of HAPIs and implement Rivera’s PIP bundle to reduce the HAPIs incidence rates within the critical care unit with 371 beds. The project considered patients in critical care units because they are at an increased risk for the development of HAPIs because of prolonged confinement in beds, hemodynamic instability, mechanical ventilation, sedation, immobility, as well as vasopressors (Kazemi et al., 2018). HAPIs tend to extend a negative impact to the patient/family experience, patient outcomes, cost of treatment, and nurse satisfaction. They result in an extended hospital stay that creates many other issues in the treatment process. The unit and the WOC nurses were encouraged to implement the PIP bundle to address the rising incidences of HAPIs in the adult critical care unit. Inconsistencies were noted during the root cause analysis in the PIP strategies.
Summary of Findings and Conclusion
To what degree does the implementation of Rivera’s PIP bundle impact the HAPI incidence compared to current practice among critical care patients in a 13-bed unit in urban New York over four weeks?Implementing the bundle influenced a decline in HAPIs for patients in the critical care unit. A 33% HAPI reduction was noted in the post-intervention stage upon implementation of the pressure injury intervention bundle over the four weeks. Pre-intervention injuries included unstageable pressure and stage 2 pressure injuries. HAPI locations were the sacrum, ear, upper thigh, heel, ischia tuberosity, as well as on the heel. During the post-intervention period, a stage two injury was noted on the sacrum. Table 3 shows that the intervention facilitated a significant reduction of HAPI and promoted the safety of patients in critical control units. There was reduction in stage I and stage II HAPIs as expected since this project was aimed only for four weeks.
The reduction influenced beneficial impact to nurses and improved their job satisfaction and patient outcome. The bundle was implemented in the critical care unit, and measures were established to ensure its sustainability. Stakeholders were encouraged to remain vigilant and determined in the prevention of HAPI.
Implications
The results of the project are likely to encourage the adoption of a PIP bundle in critical care settings to hinder HAPIs and hospitals need implement the bundle to promote patient outcomes and offer better healthcare services. The DPI project results show that nursing theories are beneficial in guiding education and research, influencing better patient care, improving communication between nurses, and better professional status. Practically, it implies that the PIP bundle can be applied to a critical care unit setting to limit the chances of the development of HAPIs. It shows that better nursing outcomes would be achieved in the future due to improved research and implementation of EBP initiatives.
Guidelines for clinical practice can offer a starting point for the implementation of the PIP bundle. The study findings show that nurses knew beneficial preventive interventions. They were expected to apply basic interventions based on the provided guidelines to facilitate the effective implementation of the PIP bundle.
The need for explicit documentation is another practice implication noted from this EBP initiative. It is necessary to assess the skin status during the admission process and ensure that it is monitored closely. It is important to consistently document interventions for both the treatment and prevention of HAPIs. Documentation is necessary for legal and economic perspectives since PIP interventions are sometimes costly. Poor documentation can influence denial or reduction of reimbursement implying that it is important to ensure it is properly done. Insufficient documentation has influenced many medical liability allegations to go to trials and eventually face charges. Daily flow sheets and admission assessment forms can help staff nurses to promote documentation.
The aim of every research work, especially in the medical field, is to find a solution to a problem or spearhead potential change that can improve service delivery. As such, the primary purpose of the current project was to offer a possible solution to the issue of HAPIs. These are a real threat to the American healthcare system. The problem mostly affects patients receiving care in the critical care units. The aged, particularly exhibit increased HAPIs risk because of their vulnerable skin cells. Therefore, the findings that Rivera’s PIP bundle can cause positive effect to the HAPIs’ frequency are great news to the American healthcare and academia fraternity. The results of the study thus lead to several implications. The discussion below tackles the theoretical, practical, and future implications of the study’s findings.
Theoretical Implications
The project involved practice improvement which aligns with various nursing theories concerning evidence-based nursing practice. Jean Watson’s human caring theory (2018) identifies how to improve positive outcomes during human-to-human caring moments. Wei and Watson (2019) indicate that the theory relies on practice, research, and theory-based education to ensure that any proposed intervention is suitable and can help patients achieve better health outcomes. Watson’s theory of caring helps create an excellent environment around the patients and staff to promote healing. Energetic authentic caring presence occurs when the nurse and patient come together to create a caring moment. Pressure injuries occur mostly in immobile and elderly patients and PIP bundle interventions, performed by the nurse or the healthcare team, such as repositioning an immobile patient can prevent pressure injuries, meet the basic needs of patient, and help sustain human dignity. The human caring nursing theory promotes healing and encourages the provision of a favorable healing environment. The theory encourages nurses to put their patients in the best environment to support their healing process. Active engagement in the caring process through intentionality and authentic presence enabled nurses to promote the ability of patients to recover. It improved the ability of nurses to maintain caring attitudes and emotional sensitivity, particularly when working in a demanding and over-stressed workplace. It potentiates capabilities and regenerates life energies to motivate nurses to offer the best service in critical care units. During the implementation of PIP bundles, the theory promoted self-actualization both personally and professionally. It motivated nurses to implement the PIP bundle to reduce incidences of HAPIs among adults in CCU. The theory was applied to improve patient satisfaction and encourage nurses to develop a positive attitude towards their patients and the environment. It promoted quality caring and influenced the implementation of the PIP bundle while enhancing patients’ experiences.
Practical Implications
Practice improvement can enhance job satisfaction, patient experience and promote the nursing outcome. It can play a role in the reduction of the cost of treatment and lower the hospital stay. It can motivate nurses to work harder and remain focused on the achievement of their expectations. This can help solve the problem of a poor attitude towards the job and ensure that everyone is focused on the improvement of patients’ safety. Further research in the PIP bundle is likely to influence the better outcome and facilitate the achievement of the nursing objectives.
Nurses caring for patients particularly those in high-risk settings need to understand risk factors associated with the development of HAPIs and interventions necessary to enhance control. They need to be educated on key areas such as risk factors, prevalence and incidence, documentation, preventative interventions, patient education strategies, risk assessment scales, prevalence, and incidences.
Clinicians need to make an effort to identify patients who are at an increased risk of developing pressure. They need to consider risk factors such as cognitive impairment, lower body weight, Hispanic ethnicity, older age, and physical impairments. Patients with other comorbid conditions affecting the healing process and the integrity of the soft tissues such as impaired microcirculation, edema, diabetes, malnutrition, hypoalbuminemia, and fecal incontinence are exposed to the risk of developing pressure ulcers. Individualized decisions are necessary to determine whether to use a multicomponent or single intervention to hinder the development of pressure ulcers.
Future Implications
The project revealed that the PIP bundle can offer a solution to the problem of HAPIs among adult patients in the critical care unit. This means that implementation of the PIP bundle is likely to transform the delivery of health services to patients in critical units. Reduction in the prevalence of pressure ulcers would promote patients ‘experience, reduce the cost of treatment and enhance job satisfaction among nurses. Future DPI projects are likely to focus on improved interventions meant to boost the implementation of the PIP bundle and enhance its relevance in critical care settings. They are likely to consider measures to boost the motivation of nurses and improve their ability to collaborate with other practitioners. The other implication is that the DPI project would be implemented in critical care units and not in other units. This is because it was conducted in a unit where adult patients were confined in the hospital beds for a prolonged period.
Recommendations
Findings from the present project reveal the essence of Rivera’s PIP bundle in managing HAPIs cases in critical care units. It is clear from the study that adopting the PIP initiative stands to improve the current situation in the U.S. hospitals and the healthcare system at large. Nonetheless, several takeaways ought to be appreciated for the PIP bundle to work well. The present recommendations thus find their basis on the findings and the settings of the project. For instance, the use of PIP bundle to manage HAPIs needs hospitals and critical care facilities to ensure the availability of the right number of nurses in the facilities. The aspect leads to the realization of the appropriate nurse to patient ratio, which promotes the intervention’s effectiveness. From the project, a nurse to patient ration of one (nurse) to three (patients) stands to deliver some optimum results. The best ratio would, however, be one nurse for each specific patient, especially, in the critical care units. The point that America lacks the capacity to realize such a ration thus leads to the recommendation that the nation and individual hospitals needs to improve the number of employed nurses for the positive results to be realized.
Better still, the PIP bundle initiative not only requires hospitals to have the right nurse to patient ratio, but also to exhibit highly skilled nurses with the intrinsic motivation to promote quality care. A major part of the present project’s methodology phase involved the selection and training of both wound and data entry nurses for the project. The wound nurses required basic training on issues like incidence reporting and recording, while the data management nurses received training on the administration of the PIP bundle intervention. Close supervision from the research teams was also necessary to ensure that the utilized wound nurses implemented the new skills. The training and close supervision facets thus aided greatly in the realization of the acquired results that promise the effectiveness of the PIP bundle tactic in managing HAPIs.
As such, it is of great importance that hospitals purposing to employ the intervention under study implements such basic factors to enjoy similar outcomes. Such is to imply that hospitals have to incur more costs to benefit from PIP bundle intervention. The average American crical care unit, for example, requires to hire at least ten wound nurses to comply with the nurse to patient ratio requirement suggested by the present study. Moreover, the acquisition of an effective EHR system is also vital for all the facilities intending to benefit from the suggested intervention. All these, plus several other aspects, makes the PIP bundle strategy a highly reliable but somewhat costly intervention for many facilities. However, the point that one of the healthcare’s primary purposes to save life makes the cost issue significantly negligible, especially now that a possible solution to HAPIs, which cost America billions of dollars, is out. The intervention is worth every cent and needs to be implemented to save the situation.
Recommendations for Future Projects
The findings of the present research work provide direction for both registered nurses involved in critical care and the professional nurses intending to further investigations regarding the issue of HAPIs. As such, future scientific projects should evaluate the outcomes of the Rivera PIP bundle implementation while paying attention to factors such as quality of care, cost, and motivation for nurses. A possible way to undertake future studies on this topic include the utilization of more quasi-experimental designs to test, describe, and explain the relationship between outcomes, interventions, and risks of associated with the new intervention. Quasi-experimental studies exibit the potential to support the development of better interventions to assist more patients in critical care units.
Future projects also need to analyze the cost-benefit in the preventative intervention to justify its application in critical care units. This should include the analysis of the cost, benefits, and challenges associated with the PIP implementation. It is necessary to determine the actual cost and consider the obtained benefits to justify the implementation of the PIP bundle. Benefits analyses need to be conducted on ulcer development and preventive interventions. This can help offer evidence of potential benefits against the associated costs with the bundle implementation. Evaluated benefits should include savings on the treatment process, quality of care, patients’ satisfaction, and employee morale. The research would support the effective making of decisions when caring for patients in critical care units.
Further research is necessary to determine the comparative efficacy of different pressure ulcer risk assessment tools as well as compare it with clinical judgment. Limited studies exist on the efficacy of interventions warranting more researches. This can improve the ability of nurses and others health practitioners to make informed decisions regarding the best interventions to apply based on the patient’s condition. This can play a role in the reduction of the cost of treatment and promote the quality of care to patients. It would boost the knowledge of health providers and improve their understanding of issues affecting their patients.
Future DPI projects need to evaluate the impact of the PIP bundle implementation on the educational and skills needs of nurses. Since the EBP initiative incorporates diverse disciplines and encourages the application of diverse interventions, it is necessary to determine whether higher education would be necessary. The research needs to provide an answer to whether critical skills would be necessary to meet the new requirements. This will also determine whether the skills of nurses in the current practice are sufficient to support the bundle implementation.
More research is also necessary to determine whether the bundle can be implemented in other setting apart from critical care units. The research needs to determine changes that can be done in the bundle to fit and remain effective in different places. This is important to increase the number of patients benefiting from the DPI project. The research needs to determine measures that can be taken to motivate nurses and enhance their commitment.
Recommendations for Practice
This project recommends further documentation of HAPIs in critical care units to understand changing needs of the population. Documentation is important for improved clinical communication ensuring that information is shared appropriately. Further documentation of HAPIs would offer an accurate reflection of patient safety, explain the need for nursing assessments, and improve the ability of the multidisciplinary team to offer quality care. Accurate documentation would offer evidence of care, legal requirements and support effective decisions. It would ensure consistent communication enabling every nurse to offer the best quality service.
The development of a PIP checklist can help promote adherence to the provided guidelines. The checklist can support the documentation of the number and types of the implemented preventive interventions. It can offer guidance to nurses during their practice and improve the patients’ experience. It would standardize the process enabling the consideration of all actions and elements. The predictability and structure of the checklist would support systematic and careful delivery of care to enhance performance while lowering variability. It would support the delivery of quality, safe, and evidence-based best practices by ensuring that every patient receives evidence-based care and democratizing knowledge. The checklist would support the implementation of a formalized process, eliminate inconsistent procedures, and reduce chances of errors. It would support the adoption of effective interventions to influence the achievement of a better outcome. To ensure success of the PIP bundle intervention, it is essential to adhere to the established guidelines and ensure that every detail is followed.
The other recommendation is to train new staff in the large-scale PIP Bundle implementation and ensure that they have the right skills. Training would ensure that nurses develop the right skills required to support the successful implementation of the bundle. This can play a role in the motivation of nurses and other health practitioners to offer the best services to their patients and enhance adherence to the bundle. Providing them with the right knowledge would ensure that everyone understands the need of implementing the PIP bundle and remain committed to the delivery of quality care.
References
Adashi, E. Y., Walters, L. B., & Menikoff, J. A. (2018). The Belmont Report of 40: Reckoning with time. American Journal of Public Health, 108(10), 1345-1348. doi:10.2105/AJPH.2018.304580
Aljezawi, M., & Tubaishat, A. (2018). Pressure injuries among hospitalized patients with cancer. Journal of Wound, Ostomy, and Continence Nursing, 45(3), 227-232(6). doi:10.1097/WON.0000000000000429
Anderson, M. (2018). Universal Pressure Ulcer Prevention Bundle with WOC Nurse Support: A Pressure Injury Prevention Journey. In Pressure Injury, Diabetes and Negative Pressure Wound Therapy (pp. 31-41). Springer, Cham.
Bates‐Jensen, B. M., McCreath, H. E., Harputlu, D., & Patlan, A. (2019). Reliability of the Bates‐Jensen wound assessment tool for pressure injury assessment: The pressure ulcer detection study. Wound Repair and Regeneration, 27(4), 386-395.
Bell, E., Bryman, A., & Harley, B. (2018). Business research methods. London, UK: Oxford University Press.
Burnes, B. (2020). The origins of Lewin’s three-step model of change. The Journal of Applied Behavioral Science, 56(1),32-59.
Chaboyer, W. P., Thalib, L., Harbeck, E., Coyer, F. M., Blot, S., Bull, C., Nogueira, P. C., & Lin, F. F. (2018). Incidence and prevalence of pressure injuries in adult intensive care patients: A systematic review and meta-analysis. Critical Care Medicine, 46(11), 1074-1081. doi:10.1097/CCM.0000000000003366
Cheng, H., Sun, X., Ji, X., Zhang, J., Lv, J., Li, T., & Ding, L. (2020). Risk factors and the potential of nomogram for predicting hospital-acquired pressure injuries. International Wound Journal, 17(4), 974–986.
Chitambira, B., & Evans, S. (2018). Repositioning stroke patients with pusher syndrome to reduce incidence of pressure ulcers. British Journal of Neuroscience Nursing, 14(1), 16-21. doi:10.12968/bjnn.2018.14.1.16
Cornish, L. (2017). The use of prophylactic dressings in the prevention of pressure ulcers: a literature review. British journal of community nursing, 22(Sup6), S26–S32.
Courvoisier, D. S., Righi, L., Béné, N., Rae, A.-C., & Chopard, P. (2018). Variation in pressure ulcer prevalence and prevention in nursing homes: A multicenter study. Applied Nursing Research, 42, 45-50. doi:10.1016/j.apnr.2018.06.001
Cox, J., Roche, S., & Murphy, V. (2018). Pressure injury risk factors in critical care patients: A descriptive analysis. Advances in Skin & Wound Care, 31(7), 328-334. doi:10.1097/01.ASW.0000534699.50162.4e
Creswell, J. W., & Creswell, J. D. (2018).Research design: Qualitative, quantitative, and mixed methods approaches(5th ed.).Thousand Oaks: CA. Sage Publications.
Dreyfus, J., Gayle, J., Trueman, P., Delhoughe, G., & Siddiqi, A. (2017). Assessment of risk factors associated with hospital-acquired pressure injuries and impact on health care utilization and cost outcomes in US hospitals. American Journal of Medical Quality, 33(4), 348-358. doi:10.1177/1062860617746741
Eren, F., DeLuca, R., & Kirshblum, S. (2020). Frequency of turning in bed at home in persons with chronic spinal cord injury. The Journal of Spinal Cord Medicine. doi:10.1080/10790268.2020.1800965
Flannelly, K. J., Flannelly, L. T., & Jankowski, K. R. B. (2018). Threats to the internal validity of experimental and quasi-experimental research in healthcare. Journal of Health Care Chaplaincy, 24(3), 107-130. doi:10.1080/08854726.2017.1421019
Fowler, S. B., & Lapp, V. (2019). Sample size in quantitative research: Sample size will affect the significance of your research. American Nurse Today, 14(5), 61-63.
Frank, G., Walsh, K. E., Wooton, S., Bost, J., Dong, W., Keller, L., Miller, M., Zieker, K., & Brilli, R. J. (2017). Impact of a pressure injury prevention bundle in the solutions for patient safety network. Pediatric Quality & Safety, 2(2), 1-8.
Gaspar, S., Peralta, M., Marques, A., Budri, A., & de Matos, M. G. (2019). Effectiveness on hospital-acquired pressure ulcers prevention: A systematic review. International Wound Journal, 16(5), 1087-1102. doi:10.1111/iwj.13147
Gray, M., & Giuliano, K. K. (2018). Incontinence-associated dermatitis, characteristics, and relationship to pressure injury. Journal of Wound, Ostomy, and Continence Nursing, 45(1), 63-67. Web.
Greenwood, C., & McGinnis, E. (2016). A retrospective analysis of the findings of pressure ulcer investigations in an acute trust in the UK. Journal of Tissue Viability, 25(2), 91-97. doi:10.1016/j.jtv.2016.02.008
Gupta, P., Shiju, S., Chacko, G., Thomas, M., Abas, A., Savarimuthu, I., Omari, E., Al-Balushi, S., Jessymo, P., Mathew, S., Quinto, M., McDonald, I., & Andrews, W. (2020). A quality improvement programme to reduce hospital-acquired pressure injuries. BMJ Open Quality, 9(3), e000905.
Hahnel, E., El Genedy, M., Tomova-Simitchieva, T., Hauß, A., Stroux, A., Lechner, A., Richter, C., Akdeniz, M., Blume-Peytavi, U., Löber, N., & Kottner, J. (2020). The effectiveness of two silicone dressings for sacral and heel pressure ulcer prevention compared with no dressings in high-risk intensive care unit patients: a randomized controlled parallel-group trial. The British Journal of Dermatology, 183(2), 256–264.
Han, Y., Jin, Y., Jin, T., Lee, S. M., & Lee, J. Y. (2019). Impact of pressure injuries on patient outcomes in a Korean hospital: A case-control study. Journal of Wound, Ostomy and Continence Nursing, 46(3), 194-200. doi: 10.1097/WON.0000000000000528
Hultin, L., Karlsson, A.-C., Öhrvall, M., & Gunningberg, L. (2019). Information and communication technology can increase patient participation in pressure injury prevention: A qualitative study in older orthopedic patients. Journal of Wound, Ostomy, and Continence Nursing, 46(5), 383-389. doi:10.1097/WON.0000000000000568
Jager, J., Putnick, D. L., & Bornstein, M. H. (2017). More than just convenient: The scientific merits of homogenous convenience samples. Monographs of the Society
Joint Commission. (2016). Preventing pressure injuries [PDF document]. Web.
Kamikawa, N., Hamada, H., Sekikawa, K., Yamamoto, H., Fujika, Y., Kajiwara, T., Aizawa, F., & Otoyama, I. (2018). Posture and firmness changes in a pressure-relieving air mattress affect cough strength in elderly people with dysphagia. PLOS ONE, 13(12), e0208895.
Kayser, S. A., VanGilder, C. A., & Lachenbruch, C. (2019). Predictors of superficial and severe hospital-acquired pressure injuries: A cross-sectional study using the International Pressure Ulcer Prevalence™ survey. International Journal of Nursing Studies, 89, 46-52.
Kazemi, A., Carnaggio, K., Clark, M., Shephard, C., & Okoye, G. A. (2018). Optimal wound care management in hidradenitis suppurativa. Journal of Dermatological Treatment, 29(2), 165-167.
Kennerly, S. M., & Yap, T. L. (2018). The role of manual patient turning in preventing hospital acquired conditions. California: Leaf Health Care.
Kim, C. G., Park, S., Ko, J. W., & Jo, S. (2018). The relationship of subepidermal moisture and early stage pressure injury by visual skin assessment. Journal of Tissue Viability, 27(3), 130-134.
Latimer, S., Chaboyer, W., Thalib, L., McInnes, E., Bucknall, T., & Gillespie, B. M. (2019). Pressure injury prevalence and predictors among older adults in the first 36 hours of hospitalisation. Journal of Clinical Nursing, 28(21-22), 4119-4127. Web.
Lewin, K. C. (1951). Field theory in social science. New York, NY: Harper & Row.
Li, Z., Lin, F., Thalib, L., & Chaboyer, W. (2020). Global prevalence and incidence of pressure injuries in hospitalized adult patients: A systematic review and meta-analysis. International Journal of Nursing Studies, 105(103546), 1-13. doi:10.1016/j.ijnurstu.2020.103546
Lim, M. L., & Ang, S. Y. (2017). Impact of hospital-acquired pressure injuries on hospital costs – experience of a tertiary hospital in Singapore. Wound Practice & Research: Journal of the Australian Wound Management Association, 25(1), 42-47.
Lin, F., Wu, Z., Song, B., Coyer, F., & Chaboyer, W. (2020). The effectiveness of multicomponent pressure injury prevention programs in adult intensive care patients: A systematic review. International Journal of Nursing Studies, 102. doi:10.1016/j.ijnurstu.2019.103483
Luo, M., Long, X.-H., Wu, J.-I., Huang, S.-Z., & Zeng, Y. (2019). Incidence and risk factors of pressure injuries in surgical spinal patients: A retrospective study. Journal of Wound, Ostomy, and Continence Nursing, 46(5), 397-400. doi:10.1097/WON.0000000000000570
Mansfield, S., Obraczka, K., & Roy, S. (2019). Pressure injury prevention: A survey. IEEE reviews in biomedical engineering, 13, 352-368.
Padula, W. V., & Delarmente, B. A. (2019). The national cost of hospital-acquired pressure injuries in the United States. International Wound Journal, 16(3), 634-640.
Padula, W. V., & Pronovost, P. J. (2018). Addressing the multisectoral impact of pressure injuries int the USA, UK, and abroad. BMJ Quality & Safety, 27(3), 171-173. doi:10.1136/bmjqs-2017-007021
Padula, W. V., Black, J. M., Davidson, P. M., Kang, S. Y., & Pronovost, P. J. (2020). Adverse effects of the Medicare PSI-90 hospital penalty system on revenue-neutral hospital-acquired conditions. Journal of Patient Safety, 16(2), e97-e102. doi: 10.1097/PTS.0000000000000517
Padula, W. V., Pronovost, P. J., Makic, M. B. F., Wald, H. L., Moran, D., Mishra, M. K., & Meltzer, D. O. (2019). Value of hospital resources for effective pressure injury prevention: A cost-effectiveness analysis. BMJ Quality & Safety, 28(2), 132-141. doi:10.1136/bmjqs-2017-007505
Razmus, I., & Bergquist-Beringer, S. (2017). Pressure injury prevalence and the rate of hospital-acquired pressure injury among pediatric patients in acute care. Journal of Wound, Ostomy, and Continence Nursing, 44(2), 110-117. doi: 10.1097/WON.0000000000000306
Ricci, J. A., Bayer, L. R., & Orgill, D. P. (2017). Evidence-based medicine: The evaluation and treatment of pressure injuries. Plastic and Reconstructive Surgery, 139(1), 275e-286e. doi:10.1097/PRS.0000000000002850
Rivera, J., Donohoe, E., Deady-Rooney, M., Douglas, M., & Samaniego, N. (2020). Implementing a Pressure Injury Prevention Bundle to Decrease Hospital-Acquired Pressure Injuries in an Adult Critical Care Unit: An Evidence-Based, Pilot Initiative. Wound Management & Prevention, 66(10), 20-28.
Romanelli, M., Clark, M., Gefen, A., & Ciprandi, G. (Eds.). (2018). Science and practice of pressure ulcer management (2nd ed.). Springer Nature.
Rutberg, S., & Bouikidis, C. D. (2018). Focusing on the fundamentals: A simplistic differentiation between qualitative and quantitative research. Nephrology Nursing Journal, 45(2), 209-212.
Shi, C., Dumville, J. C., & Cullum, N. (2018). Skin status for predicting pressure ulcer development: a systematic review and meta-analyses. International Journal of Nursing Studies, 87, 14-25.
Siedlecki, S. L. (2020). Quasi-experimental research designs. Clinical Nurse Specialist, 34(5), 198-202. doi:10.1097/NUR.0000000000000540
Singh, C. D., Anderson, C., White, E., & Shoqirat, N. (2018). The impact of pediatric pressure injury prevention bundle on pediatric pressure injury rates. Journal of Wound, Ostomy and Continence Nursing, 45(3), 209-212.
US Department of Health & Human Services. (1979). The Belmont report.
Watson, J. (2018). Unitary caring science: The philosophy and praxis of nursing. Louisville, CO: University Press of Colorado.
Wei, H., & Watson, J. (2019). Healthcare interprofessional team members’ perspectives on human caring: A directed content analysis study. International Journal of Nursing Sciences, 6(1), 17-23. doi:10.1016/j.ijnss.2018.12.001
World Health Organization. (2008). Summary of the evidence on patient safety: implications for research. Geneva, Switzerland: WHO Press.
Yafi, A., Muakkassa, F. K., Pasupneti, T., Fulton, J., Cuccia, D. J., Mazhar, A., Blasiole, K. N., & Mostow, E. N. (2017). Quantitative skin assessment using spatial frequency domain imaging (SFDI) in patients with or at high risk for pressure ulcers: QUANTITATIVE SKIN ASSESSMENT USING SPATIAL FREQUENCY. Lasers in Surgery and Medicine, 49(9), 827-834.
Appendix A
Appendix B
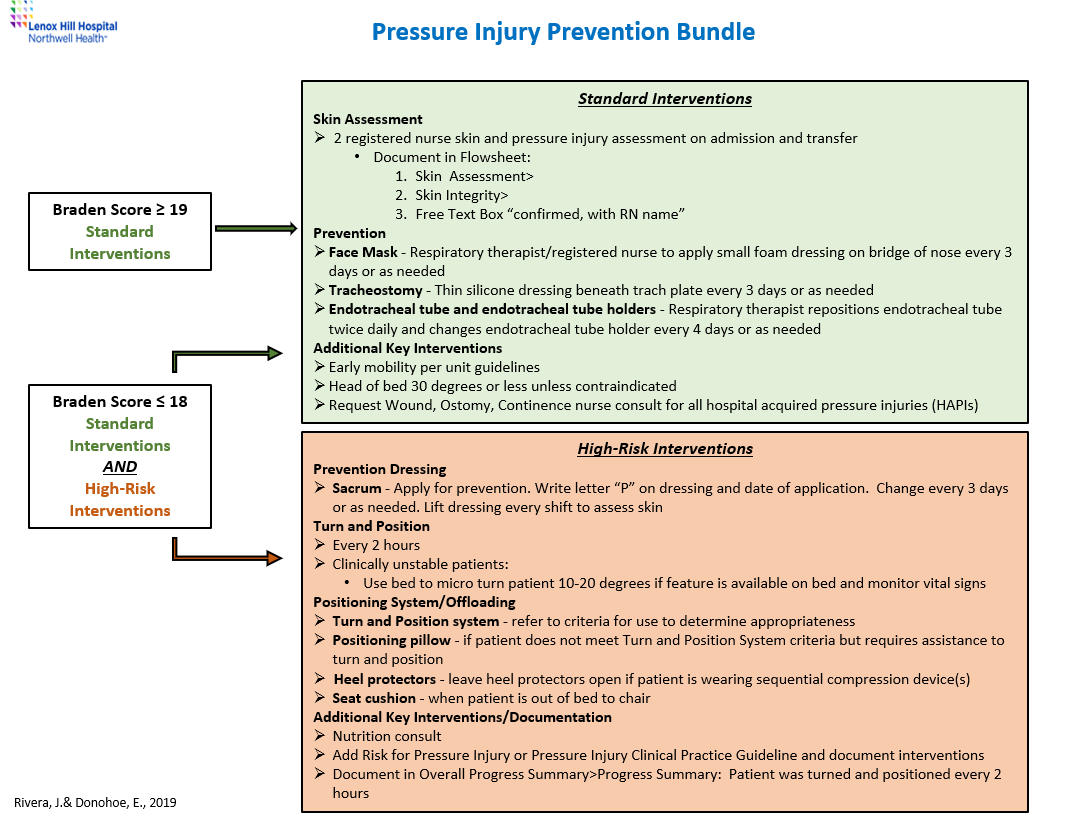
Appendix C