HIPAA
Rules which dictate how health information should be used and who should access it.
Protects patients and covered entities along with their business associates.
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) includes a set of rules that seek to protect patients’ health information by controlling its disclosure and use. Hence, it protects the patient from harm by third parties, and covered entities and their business associates from costly litigation procedures. For example, for employed individuals, when certain information is revealed, it might jeopardize their career; hence, can readily sue the responsible institution. HIPAA is important to front office staff in guiding their demeanor when handling and communicating patient health information (Office for Civil Rights, 2013).
They should use general language when addressing clients, such as, your payment method instead of your insurance. They should also keep their screen and patient documents away from others, other than the front-office staff or authorized party, for instance, other healthcare workers.
Relevance of HIPAA
Front-office Staff
- Discretion when handling
- patient information
Nurses
Should not readily disclose patient information
Clinicians
Should not reveal their patients’ health information publicly
Nurses and physicians should not disclose patient health information as they usher in patients to examination rooms or when discussing procedures and their conditions with them. They should maintain low voices with other healthcare workers or patients when talking about a patient’s condition. They should not leave patient documents lying around in a manner that can be easily read by others. Hence, any document with patient health information should be handled with discretion, and discussions of patients care processes should be done in private spaces. Clinicians should make sure that patients are only accompanied to the examination room if they allow it. Additionally, they should not disclose their patients’ treatment plan without their consent. They should not present and discuss diagnosis and treatment plans in public.
How to Communicate with Patients in Compliance with HIPAA
- Encryption when using the email
- Discretion with written information
- Confidentiality
- Routine provision of patient health information is not necessary
While communicating with patients, either verbally or written, it is important to ensure that the right mechanisms are in place. In the case of mails, for example, it is important for the emails to be encrypted such that even if they are intercepted, the contents cannot be accessed by third parties. Moreover, these emails should not contain a patient’s health information because intruders might bump into them. Hence, by refraining from using patient information, intruders cannot trace the patient. Patient information should be kept confidential and not revealed to a third party. When discussing patient information, it should be within closed doors, and when sending information to the patient through email, it should be encrypted to avoid access by a third party. Routine provision of patient health information is not necessary unless in special circumstances.
Communicating PHI
- Over the phone
- Distance from the client being served and others
- Speaking in a low tone that is not heard by others
- Talking with a patient in a private area
PHI includes identifiers from demographic and socio-economic data through which an individual can be identified and traced.
Thereby, it is essential to limit the disclosure and use of PHI in the presence of unauthorized third parties, but when needed, discretion and confidentiality should be the guiding principles by adopting the specific practices mentioned in this slide (Kulwicki, 2015). When communicating PHI, it should be over the phone in certain circumstances, for example, when confirming appointment details, as it prevents linking particular information to a patient. Institutions should ensure to maintain adequate distance between the client being served and others. Healthcare providers should talk in a low tone that is not heard by others. When discussing issues with patients, it should be in a private area away from other unauthorized parties.
HIPAA Breaches
- Accessing patient health information for non-health related reasons
- Not carrying out a regular risk analysis to sure PHI is secure and well-protected
- Speaking/discussing a patient’s situation when other unauthorized or irrelevant individuals are around
Lack of a privacy officer
A HIPAA breach occurs when an organization does not have proper measures in place to ensure that its patient health information system is free from the risk of unauthorized access. As a result, various mistakes which constitute HIPAA breaches occur which include not carrying out a regular risk analysis to sure PHI is secure and well-protected. Speaking/discussing a patient’s situation, when other unauthorized or irrelevant individuals are around, is another breach. Lack of a privacy officer within an organization to ensure that the right protocols and procedures are in place as per the HIPAA rules, and all staff adhere to them (Schwartz, 2016). Additionally, accessing patient health information for other reasons other than operations related to healthcare and associated payment procedures constitutes another breach.
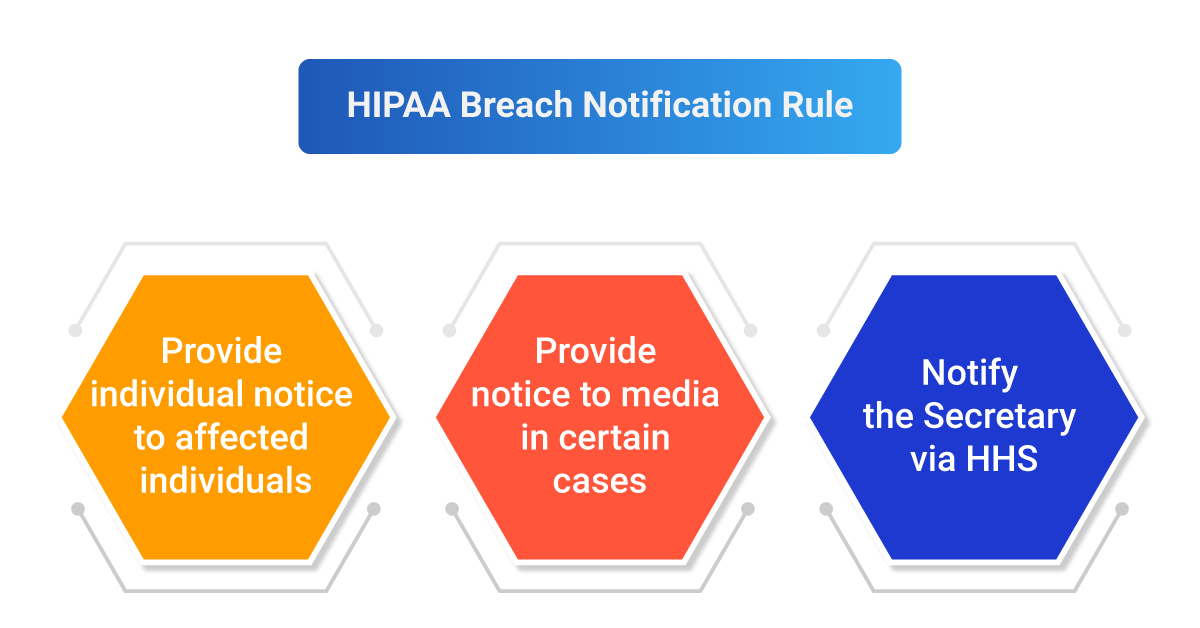
Breach Notification Requirements
Once a breach has occurred, the person with a complaint should be directed to the security officer immediately as the person mandated to oversee compliance with HIPAA. Effective communication with the person complaining helps the parties involved to reach an amicable settlement. There should be an elaborate written process for complaints that can be channeled to the relevant stakeholders within the required timeframe of 60 days (Office for Civil Rights, 2013). There should be a notification to the patient within 60 days, another one to the media in 60 days, and an additional one to the secretary or covered entity if happening at the setting of a business associate. Moreover, there should be an elaborate written process for complaints.
Patient Protection Regulations Relevant to Healthcare Organizations
- HIPAA
- ACA
- CDC
- CMS
- FDA
The overall goal of the patient protection regulations is to ensure that populations receive quality healthcare services and associated procedures as well as safe and acceptable consumables. First, there is the HIPAA rule through which patient safety is achieved by protecting the use and disclosure of patient health information. Then there is the affordable care act (ACA), which asserts the need to ensure that all Americans receive effective health and human services as per the mission of the U.S. Department of Health and Human Services. The CDC advocates for preventive health while the Center for Medicare and Medicaid Services (CMS) asserts the need for cost-effective and advanced health while the FDA ensures products for use and consumption are up to standard to avoid harm.
- Informed Consent
- Informed consent-patient fully understands the available care options in terms of their benefits and risks
Provider’s Role
- Developing a healthy relationship with the client
- Avoiding presenting long and detailed informed consents
- Conveying all relevant information in a clear and precise manner
Informed consent is essential when considering the available care options and which to implement as it enables a patient to choose a treatment aligned to their values after comprehending the care options involved. Informed consent is when a patient fully understands the available care options in terms of their benefits and risks; thereby makes a decision on the preferred option once they fully understand the involved procedures. The provider is expected to be clear and precise when relaying information about the procedure and should not leave out any details based on a healthy relationship with the patient. The patient, on the other hand, should read an informed consent thoroughly or ask the healthcare provider or someone accompanying them to read it out to them and ask questions where they do not understand (Stunkel et al., 2010).
Patient’s Role
- Reading the informed consents thoroughly
- Asking questions where they do not understand
Importance of Adhering to Regulations
- To prevent potential harm
- To avoid costly litigation procedures
- To receive rewards
When various regulations seeking to protect patients from malicious activities are adhered to, patient health information flows across authorized persons seeking to deliver quality care, and patients, as well as healthcare providers, do not have to go through hectic and costly litigation processes. Instead, they are rewarded in the form of merit-based incentives and advance alternative payment (Health IT legislation, 2020).
Recommendations
- Staff training
- Security officer as a watchdog
- Conducting regular risk assessments
- No need for healthcare providers to disclose patient information on a regular basis
Ensuring that all staff members are empowered by the HIPAA rule and associated patient protection regulations is fundamental as a precedent for the delivery of quality and safe healthcare. Moreover, confidentiality and limited exposure of patient information are paramount through the installation of efficient systems. Regular risk assessments can help to identify potential breaches. All the staff should be trained on the HIPAA and the practices they need to adopt to attain compliance. There should be a security officer in place to act as a watchdog in ensuring that everyone adhered to the HIPAA. Conducting regular risk assessments to identify gaps in the security systems before any breach occurs is imperative. There is no need for healthcare providers to disclose patient information on a regular basis; even calling out patient’s names is not ideal, and codes can be used instead (Schwartz, 2016).
References
Health IT legislation. (2020). Web.
Kulwicki, B. S. (2015). It’s five o’clock; do you know where your records are: Obligations of individuals and entities to secure protected health information. SMU Science and Technology Law Review, 18(4), 455-480.
Schwartz, S. K. (2016). 10 HIPAA mistakes practices must avoid: A breach or poor audit result can undo years of a physician’s hard work. Web.
Stunkel, L., et al. (2010). Comprehension and informed consent: assessing the effect of a short consent form. IRB, 32(4), 1–9.
Office for Civil Rights. (2013). HIPAA for professionals. Web.