Abstract
Chronic obstructive pulmonary disease (COPD) is a severe condition affecting the lungs and an individual’s ability to breathe, commonly resulting in hypoxemia. One of the most common practices in clinical settings during acute exacerbations of COPD is oxygen therapy for short-term effects in maintaining oxygen blood saturation at appropriate levels. Guidelines, although scarce, generally support the practice and both research and anecdotal evidence suggests that supplemental O2 is effective in reducing hypoxemia and therefore, decreasing morbidity and mortality in acute COPD. This paper explores the background and history of oxygen therapy, guidelines and common procedures of its application in COPD, and critically analyzes evidence on the topic. In answering the research question of whether supplemental O2 is safe and effective in the treatment of acute exacerbations of COPD, the evidence suggests that it is an effective procedure that provides first-line emergency treatment to the patient but should be used in combination with other appropriate medication and patients must be continuously monitored to avoid oxygen-related adverse events.
Introduction
Chronic obstructive pulmonary disease (COPD) is a prevalent chronic disease characterized by inflammation of the lungs and obstructed airflow which presents with symptomatic breathing-related issues such as resting hypoxemia, wheezing, and coughing. COPD is diagnosed by any combination of chronic bronchitis, emphysema, or COPD, with approximately 16.4 million people (6.6% of adults) confirmed with at least one type of COPD in the United States (American Lung Association, 2019). One of the most common interventions for COPD is the use of supplemental oxygen, which can be administered by nurses. The premise is that supplemental O2 helps alleviate hypoxic respiratory drive causing hyperventilation and increase oxygen saturation which is likely below normal thresholds in COPD patients. This paper will focus on the use of supplemental oxygen in exacerbated COPD cases. The research question is: Is the use of supplementary oxygen therapy warranted in COPD patients for acute treatments?
Background
Oxygen therapy otherwise known as supplemental oxygen (O2) is a common procedure utilized in hospitals, medical settings, and can even be set up at home through prescription. Oxygen is the most commonly used drug in emergency medicine for the treatment of symptoms of hypoxemia. The laboratory discovery of oxygen occurred in 1771 by the German-Swedish pharmaceutical chemist Carl W. Scheele. The value of oxygen in medicine was recognized soon after its discovery. Thomas Beddoes, who is viewed as the founder of respiratory therapy, began using supplemental O2 in 1798 to treat patients with asthma and congestive heart failure. Early 20th century saw further developments of the practice and technology, including tubing for catheters and predecessors to modern-day oxygen masks. Haldane, who created the Haldane effect (measuring oxygen content in blood), and Alvan Barach are primary contributors to creating oxygen delivery systems that are the basis of modern technology used today ranging for adjustment of oxygen concentrations to maintaining positive airway pressure. The late 20th century saw mass adoption of supplemental O2 in medical practice around the world as well as evolvement of long-term oxygen therapy used for chronic COPD as more modern studies emerged in support of the practice (Heffner, 2013).
Current Standards of Practice
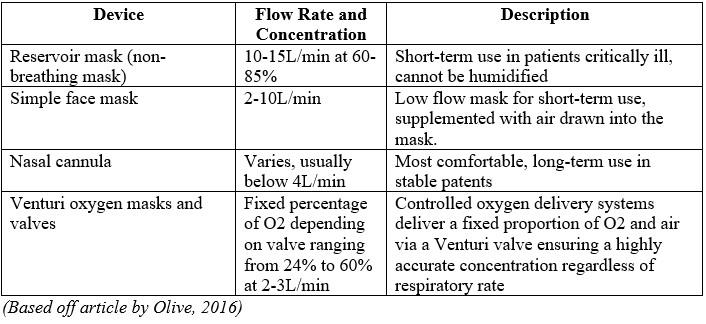
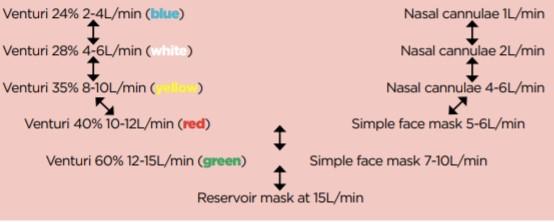
Supplemental O2 is prescribed to patients when there is a registered case of hypoxemia. The oxygen does not treat breathlessness if the patient is not hypoxic. Upon beginning oxygen therapy, a target saturation range should be prescribed (94-98% commonly) and monitored to avoid hypercapnia and minimize risk of respiratory acidosis. Pulse oximetry must be available in all settings where emergency oxygen is used. Oxygen is stored in specialized containers available in medical facilities and can be delivered via variable performance or fixed-performance devices (seen in the table below). Oxygen saturation levels are consistently monitored along with other indicators. Oxygen is titrated according to indicators and saturations (as seen in the diagram below), with patients gradually weaned off oxygen since sudden withdrawal can result in rebound hypoxemia (Olive, 2016).
COPD is an inherently complex condition, so treatments may vary significantly based on unique characteristics of the patient and context. Alongside oxygen therapy discussed, recommendations include medications such as corticosteroids and antibiotics. However, the use of supplemental O2 is one of the most common practices for patients exhibiting acute exacerbations of COPD. The Centers for Disease Control and Prevention direct to the Global Initiative for Chronic Obstructive Lung Disease for guidelines on treatment and practice. Their 2020 report indicates that in the management of moderate, severe, and life-threatening COPD exacerbation, after the severity of symptoms and blood gases are assessed, supplemental oxygen therapy should be administered for respiratory support. There are three types of respiratory support:
- Oxygen therapy – a critical, most common component of hospital treatment, supplemental O2 should be titrated to improve patient’s hypoxemia with a target saturation of 88-92% (Global Initiative for Chronic Obstructive Lung Disease, 2020). Once started, blood gases should be checked regularly to avoid rises of CO2 and PH. Venturi masks offer the best accurate and controlled delivery of oxygen at 24-28% (Currie & Douglas, 2006).
- High-flow oxygen therapy – nasal delivery of heated and humidified oxygen via specialized devices (Vapotherm) of rates up to 60 L/min in adults. HFO is a good alternative to oxygen therapy or non-invasive positive pressure ventilation.
- Ventilatory support – Utilized in emergency cases where a patient is admitted to respiratory care or intensive care (ICU). It can be provided through non-invasive (nasal/facial mask) or invasive (orotracheal tube) mean and requires specialized equipment and personnel (Global Initiative for Chronic Obstructive Lung Disease, 2020).
Supporting Evidence
Acute exacerbations of COPD are key adverse events which lead to high levels of healthcare utilization and morbidity. During the high-risk period, patients experience some level of respiratory failure. A comprehensive article by Brill and Wedzicha (2014) examines the use of oxygen therapy in acute exacerbations of COPD. The primary benefit of the procedures as it relieves the immediate hypoxia that occurs in acute exacerbations. Furthermore, supplemental O2 has been found to reduce symptoms of dyspnea both in acute and chronic COPD patients. They suggest that supplemental O2 in moderate concentrations and a monitored environment and doses is a reliable treatment to overcome hypoxia as long as the primary risk of oxygen-induced hypercarnia is avoided (Brill & Wednzicha, 2014). Similarly, Crisafulli et al. (2018) in their comprehensive overview of severe exacerbations of COPD support the use of oxygen therapy in hospitalized settings, particularly due to its effectiveness of reducing immediate mortality. While medications are potentially more effective and should be the primary form of treatment, titrated supplemental O2 provides an immediate and easy therapeutic methodology. Newer technologies such as a high flow nasal cannula with automatic adjustment devices allows for the patient to receive high flow oxygen without the CO2 retention or worsening acidosis. The authors cite several studies in support, indicating the safety and effectiveness of oxygen therapy in acute and stable COPD patients (Crisafulli et al., 2018).
Cousins et al. (2018) present the evidence of multiple authors and professional bodies that oxygen administration is viable to maintain SpO2 between levels of 88% and 92% in acute hospitalized COPD patients. The prescription of oxygen therapy helps to reduce the risk of respiratory failure in vulnerable groups. Nevertheless, they note that the prescribing practices for oxygen remain poor, despite guidelines implemented in late 2000s to inform clinician practice. However, those practices were improvement could be seen is prescribing accurate doses and measurement of pulse oximetry to ensure accurate titration (Cousins et al. 2018). It seems that despite strong evidence and guidelines, there is reluctance for oxygen therapy in some settings. Potentially, due to the dangers that supplemental O2 can present if not closely monitored, which requires either sophisticated technology or significant staff worktime. However, as noted by many of the studies, oxygen is considered a medical drug, and despite perceptions should be viewed as such. Therefore, accurate and competent use can offer great benefits, but compliance with guidelines is necessary to avoid further exacerbating the patient condition.
Meanwhile, Kane et al. (2013) identify that there is often an overreliance and lack of understanding on the use of oxygen. Up to 34% of ambulance patients and 15-17% inpatients receive oxygen at a given time, but there are very few national or international guidelines. They note that evidence suggests there is no benefit for oxygen in normoxemic or mild hypoxemia, while a common misconception of “can’t give too much oxygen” is dangerous due hyperxemia and other conditions (Kane et al., 2013). This brings up valid points as the procedure is so common, particularly in patients demonstrating shortness of breath as they would in any exacerbation of COPD, medical staff often apply oxygen therapy with relative ease with potentially lack of or even negative effects.
Conclusion
Overall, guidelines and research studies indicate that supplemental oxygen therapy is supported by strong evidence of survival benefits for acute exacerbations in COPD patients. It is appropriate to utilize in acute and clinical settings when there are clear symptoms of hypoxemia, but patients should be continuously monitored for oxygen saturation and other indicators to prevent harmful effects of supplemental O2 overuse. While oxygen therapy may be a short-term, immediate solution to a COPD crisis, that is ultimately better treated with appropriate medication, it serves a critical role in preserving organ function and overall consciousness of the patient, both of which may be affected by hypoxia induced in acute exacerbations of the disease.
References
American Lung Association. (2020). COPD prevalence. Web.
Brill, S., & Wedzicha, W. (2014). Oxygen therapy in acute exacerbations of chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease, 9, 1241-1252. Web.
Crisafulli, E., Barbeta, E., Ielpo, A., & Torres, A. (2018). Management of severe acute exacerbations of COPD: An updated narrative review. Multidisciplinary Respiratory Medicine, 13(1). Web.
Cousins, J. L., Wark, P. A., & McDonald, V. M. (2016). Acute oxygen therapy: A review of prescribing and delivery practices. International Journal of Chronic Obstructive Pulmonary Disease, 11, 1067–1075. Web.
Currie, G. P., & Douglas, J. G. (2006). Oxygen and inhalers. BMJ, 333(7557), 34–36. Web.
Global Initiative for Chronic Obstructive Lung Disease. (2020). 2020 global strategy for prevention, diagnosis and management of COPD. Web.
Heffner, J. E. (2012). The story of oxygen. Respiratory Care, 58(1), 18–31. Web.
Kane, B., Decalmer, S., & Ronan O’Driscoll, B. (2013). Emergency oxygen therapy: From guideline to implementation. Breathe, 9(4), 246–253. Web.
Olive, S. (2016). Practical procedures: Oxygen therapy. Nursing Times, 112(1/2), 12-14. Web.