Introduction
The patient and family-centered care model has occasionally come under criticism from different quarters regarding its implementation, acceptability, efficiency and awareness. For example, critics of this model have mentioned that it is difficult to implement patient and family-centered models because of the little value accorded to partnerships (between patients and families) by some societies (Johnson, 2008). The main argument here is that, traditionally, the health care sector was not keen to embrace a holistic approach to patient care and therefore, it is difficult to overcome such hurdles completely. Another criticism leveled against patient and family-centered care is the limited opportunities for educators and healthcare providers to learn and implement the model. Moreover, there have been some criticisms leveled against the model, based on the fact that there are no standards for evaluating patient and family-centered care (Johnson, 2008). In this regard, the definition of quality is also not well expanded to include patient and family centered care.
From the above criticisms of patient and family-centered care, there has been a strong need to address these inherent challenges by devising sound policies and recommendations to address the same challenges. Many organizations and healthcare institutions have come up with meaningful suggestions to address some of the criticisms leveled against patient and family-centered models. Most of these suggestions have manifested in programs and policy recommendations which have been implemented in different parts of the world. For example, among the solutions employed to solve the problem of standard recognition in patient and family-centered care is to enlist accrediting bodies when formulating standards to evaluate partnerships within the patient and family-centered model (Johnson, 2008, p. 1). Regarding the limited opportunities offered to educators and healthcare administrators (regarding the implementation and sustainability of patient and family-centered models), healthcare institutions have been advised to employ patient and family leaders in meaningful positions within the administrative system of healthcare governance (Johnson, 2008). Furthermore, regarding the little appreciation of partnership values by community members, it is advised that healthcare institutions should work with community groups to expect healthcare service provision based on partnerships and inform and convince policy makers and administrators of the importance of partnerships between patients and families (Johnson, 2008).
Most of the above recommendations and solutions have worked to solve some of the problems of patient and family centered care. For example, the initiative to convince policymakers and administrators of the importance to value partnerships with patients and family members has increased awareness regarding the roles of patients and family members in the healthcare system. Particularly, this solution has been implemented in America where a four-part national PBS series named Remaking American Medicine highlighted the successes of healthcare institutions that were able to implement parent and family centered healthcare models (Johnson, 2008). This series aired in 2006. The print media is also used to highlight the successes of patient and family centered care. For example, notable media partnerships involving the Chicago Herald, Wall Street Journal, New York Times and the Boston Global have highlighted partnerships between patients and families that are changing the healthcare sector (Johnson, 2008).
Regarding the solution to include patient and family leaders in the healthcare system, several healthcare institutions across the US have embraced this solution. For example, the Memorial Healthcare system in Florida hosts an annual conference to discuss partnerships among patients and family members (Johnson, 2008). Patient and family leaders are part of the planning team. In another initiative, the National Initiative for Children’s Healthcare Quality (NICHQ) entered into a joint partnership with the US Epilepsy foundation to improve healthcare offered to children with epilepsy – the mothers of the epileptic children were included in the planning process and constituted part of the improvement teams as well (Johnson, 2008).
The above programs have majorly borne tremendous success. However, most of such initiatives focus on improving awareness and forging partnerships with relevant stakeholders. When we compare and contrast these two methodologies, we see that programs aimed at creating awareness regarding patient and family-centered care form the ground work for future models aimed at forging partnerships. For example, through the acceptance of partnership values among healthcare administrators, patient and family leaders will be better represented in the healthcare systems. Comprehensively, through the complementary approach given to both methodologies, a high standard of efficacy is realized during the implementation of patient and family-centered models. Moreover, some of the challenges leveled against these models are effectively addressed by the same methodologies. For example, through increased awareness and collaboration of healthcare service providers and family members, opportunities to practice healthcare partnerships and sustain the same, are created. Through the understanding that effective programs and solutions can be formulated to address some of the inherent challenges of patient and family-centered care, a good plan can be formulated to address the weaknesses of patient and family-centered models. This plan is further discussed below.
Main body
“Nurses and nursing staff provide and promote care that puts people at the centre, involves patients, service users, their families and their careers in decisions, and helps them make informed choices about their treatment and care” (Manley 2011, p. 35). The above statement was made as an introduction to the role of person-centered care in the nursing practice. Its relevance to this paper is exhibited by the fact that it manifests how patient and family-centered care can be implemented in the organization by avoiding most of its inherent weaknesses. Therefore, hypothetically, to avoid the pitfalls of implementing patient and family-centered models, it is crucial to address ‘people’ concerns that make them embrace or adopt a given nursing model (McCance, McCormack and Dewing, 2011). Indeed, most of the concerns known to hinder the implementation of patient and family-centered models center on ‘people’ issues. Focusing on people issues as the main criterion for implementing patient and family-centered model is therefore a good framework for avoiding the weaknesses of adopting patient and family-centered models.
However, it should not be misunderstood that the focus on people is a substitute healthcare model for patient and family-centered care. Instead, this framework is meant to effectively tackle some of the major problems associated with incorporating patient and family centered models in the healthcare system (Smith-Stoner, 2011). For example, as explained in earlier sections of this paper, the patient and family-centered model is known to run the risk of failing to be properly embraced by all the relevant stakeholders (because of a lack of appreciation of partnership values). Focusing on people values is a solution to this problem because people tend to appreciate shared decision-making frameworks that are meant to absolve the input of all relevant stakeholders in the implementation of patient and family centered healthcare model.
Indeed, focusing on people values addresses all the inherent challenges of adopting patient and family-centered frameworks because the nursing practice is based on people as the main focus for nursing. Particularly, when focusing on a ‘person’, different factors need to be considered, such, as their engagement, cooperation, and sympathy (as just a few examples) (Manley 2011, p. 35). In addition, a person is also subject to family and community factors and therefore from this perspective, it is easy to incorporate ‘family’ elements in the nursing or healthcare practice. Person-centered models therefore provide a good wheel for implementing patient and family-centered models because they address specific people challenges. Among the basic structures of the person-centered model is engagement, having a sympathetic presence, shared decision-making, providing holistic care and working with a patient’s beliefs and values. These structures are expected to result in increased care satisfaction, increased involvement of patients and family members in healthcare decisions, increased feelings of well-being among patients and the creation of a therapeutic culture. This model is explained by the outline below:
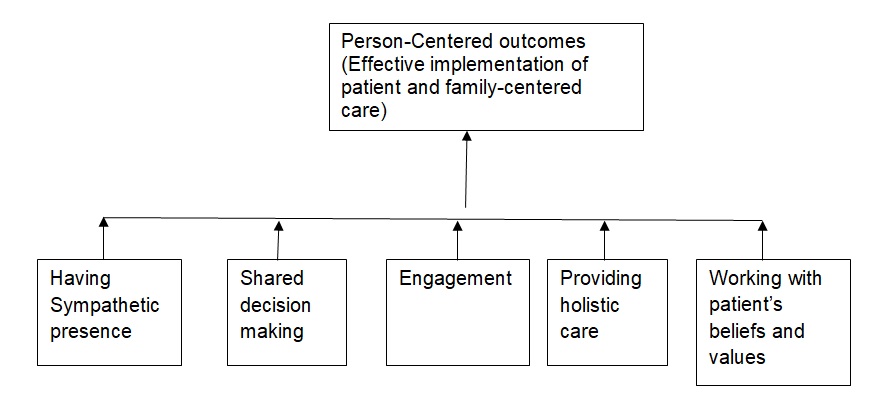
Holistically, healthcare administrators are supposed to facilitate the inclusion of family and patient leaders in the decision-making process but the bulk of the responsibility lies with the healthcare providers. In detail, nurses are required to observe that there is adequate engagement, holistic care, recognition of patients’ beliefs and values and the provision of sympathetic care to the patients.
Focusing on people as the main center for implementing patient and family-centered models is a sure way to improve the quality of care. However, this approach may still be marred by several obstacles in the realization of the expected outcomes. More importantly, the main challenge for this framework is in its sustenance. Issues of sustainability are problematic here because of detailed requirements that are needed in the implementation of the person-centered framework. For example, the implementation of this framework requires specific knowledge and skills for its proper implementation (Manley, 2011). Based on the fact that the implementation of the person-centered framework focuses on human elements, nurses are required to show different humanistic values such as dignity, respect, and compassion. However, the ability to show such humanistic elements depends on the effective practice of relationship skills (Manley, 2011). Good relationship skills also require team members to be aware of themselves and still have good interpersonal skills and other communication tools. These skills are important in assisting nurses to implement patient and family-centered models at a more personal level. Understanding patient dynamics is an important requirement for nurses but still, the way care is structured is an important contributor to the quality of healthcare provided.
Additional skills that are required in the implementation of the person-centered approach center on the professionalism and commitment of the workers towards the overall cause of the healthcare model being implemented. Referring to the commitment and professionalism of nurses in the implementation of person-centered initiatives, Manley (2011) explains that “nurses should be able to use different processes in the development of person-centered care: working with patients’ values and beliefs, engaging patients and mental health service users, having a sympathetic presence, sharing decision making and accommodating patients’ physical needs” (p. 36). Finally, it is somewhat trickier to implement people-centered initiatives on minority groups because there needs to be a careful consideration of the socio-economic dynamics of such groups. These requirements also need specialized understanding of the beliefs and values of minority groups. Therefore, the nurses and other healthcare practitioners need to be equipped with specialized skills and competencies to implement people-centered initiatives (Manley, 2011).
Another great impediment to the implementation of the people-centered framework is the lack a shared philosophy among healthcare practitioners. To properly implement the people-centered framework, it is crucial for the entire nursing team to be guided by a common philosophy. However, practically, not all nursing teams are guided by a common philosophy. The failure to work within a common philosophy stands out to be an obstacle in the implementation of people-centered frameworks because it fails to prioritize people-centered behaviors in the nursing practice. Ideally, a shared philosophy is meant to give people-centered ideologies the first priority in the nursing practice, not only to the patients but also the people around them. The welfare of the staff supposed to implement the people-centered framework is also expected to be informed by a common philosophy because sharing a common philosophy in nursing care improves the wellbeing of the staff and such an eventuality positively influences the care environment (Manley, 2011). However, there are ways to increase the prospects of shared philosophies within the nursing practice. For example, implementing person-centered frameworks where there is a supportive workplace culture is a good strategy to realizing positive outcomes (McCarthy, 2011). A supportive organizational culture will not only improve the structure and processes of people-centered initiatives but also create a common vision through which values are implemented and practiced.
Finally, another obstacle that can be witnessed in the implementation of people-centered framework is the lack of institutional support. Healthcare institutions have a big role to play in the institutionalization of person-centered frameworks because they promote user-led services. Often, desirable outcomes can be achieved by overlooking existing bureaucratic structures. These structures may include limitations on an institution’s activities because of budgetary and management concerns. Possibly, if there is no organizational support; nurses and other healthcare providers may be frustrated in implementing the people-centered framework. These frustrations usually occur from poor resourcing. It is therefore crucial to have organizational support in the implementation of people-centered frameworks because it informs the success of the initiative. One of the expected outcomes to be realized when there is enough organizational support is the allocation of enough time to initiatives that provide care through the people-centered framework. This outcome borders on quality improvement through improving the efficiency of organizations and reducing all the wastes that may be realized as a result.
Conclusion
Comprehensively, it is crucial to have all the right support structures to implement the people-centered framework because like any other healthcare model, it requires the right framework for implementation. In addition, it is crucial for an entire nursing team to be onboard; otherwise, the effort of some nurses may be undermined by the reluctance of other nurses. The importance of a supportive organizational culture also needs to be emphasized at this point. Conclusively, Manley (2011) affirms that
“The potential contribution of each member to person-centered care will be enhanced if everyone in the team is using the same approach. Such an approach requires a workplace culture where person-centered values are realized, reviewed and reflected on in relation to the experiences of both patients and staff” (p. 37).
References
Hughes, R. (2011). Overview and Summary: Patient-Centered Care: Challenges and Rewards. The Online Journal of Issues in Nursing, 16(2), 1.
Johnson, B. (2008). Partnering with patients and families to design a patient and family-centered health care system. Bethesda: Institute for patient- and family-centered care.
Manley, K. (2011). Person-Centered care: Principle of Nursing Practice D. Nursing Standard, 25(31), 35-37.
McCance, T., McCormack, B. & Dewing, J. (2011). An Exploration of Person-Centredness in Practice. The Online Journal of Issues in Nursing, 16(2), 1.
McCarthy, D. (2011). Case Study: Achieving a Culture of Patient- and Family-Centered Care at Bronson Methodist Hospital. Web.
Smith-Stoner, M. (2011). Teaching Patient-Centered Care During the Silver Hour. The Online Journal of Issues in Nursing, 16(2), 1.