Falling is a major public health issue, with outcomes ranging from minor bruising and abrasions to lacerations, fractures, head injuries, and even death. Inpatient fall and injury rates vary by unit, with medical-surgical patients at higher risk than intensive care patients. The Partnership for Patients urged acute care hospitals to explore strategies to reduce patient falls and injuries as part of the 2010 US Patient Protection and Affordable Care Act. Therefore, this paper seeks to discuss the performance improvement strategies among the care teams to help solve the issue of patient falls in surgical and medical wards.
Patient falls are a serious patient safety concern that is almost always avoidable. The following personnel would be on the Performance improvement team to investigate the fall. Registered Nursing will be at frontline to conduct or supervise accurate assessment and documentation of evaluation of fall risk factors on admission (Rosen et al., 2018). Prepared care plan tied to identified risks such as mental status, Continence, Mobility level, and Environmental risks. Supervise performance of care plan procedures or treatments such as close observation of hysterical patients, Use of assistive devices, and Maintenance of clutter-free environment. File incident report for new falls and carry out a post-fall assessment. And finally, to educate patients and families about fall risk factors.
The pharmacist will be integral in reviewing medication lists of patients at high risk based on medication profiles. Discuss medications that may increase fall risk with the physician using a standardized approach. Similarly, the patient educator will form part of the team to work with the nurse to provide appropriate educational materials and teach patients at risk for falls and their families. Facilities engineers will also participate in regularly scheduled environmental rounds to identify equipment needing repair and respond to repair requests submitted by unit staff.
Other team members include a quality officer, a nursing manager for quality and safety, and floor nursing in-charges. These personnel teams are included because there are many aspects of falls, and their causes can vary from physiological to environmental falls (Rosen et al., 2018). Therefore a mix of nursing and housekeeping personnel’s are needed to assess the patient’s risk for falls and to keep a safe environment. The mission of this practice of creating such a performance improvement team is to provide safe and quality care to patients, while the vision of is to reduce the total number of patient falls in hospitals.
Tools to Measure Falls in Patients
Checklists, goal sheets, and case analyses are examples of health care team improvement tools. They aim to improve collaboration by making team processes, goals, and case discussions more visible (Rosen et al., 2018). Standardized handoff protocols, for example, are a type of controlled team engagement, similar to a checklist, which is used to counteract information loss that occurs between care transitions (Rosen et al., 2018). These protocols promote more information interchange and improve patient, provider, and organization outcomes. This paper will use the fall reporting checklist to improve ways of dealing with patient falls in hospitals.
Fall Reporting Checklist
The 30 days investigation report
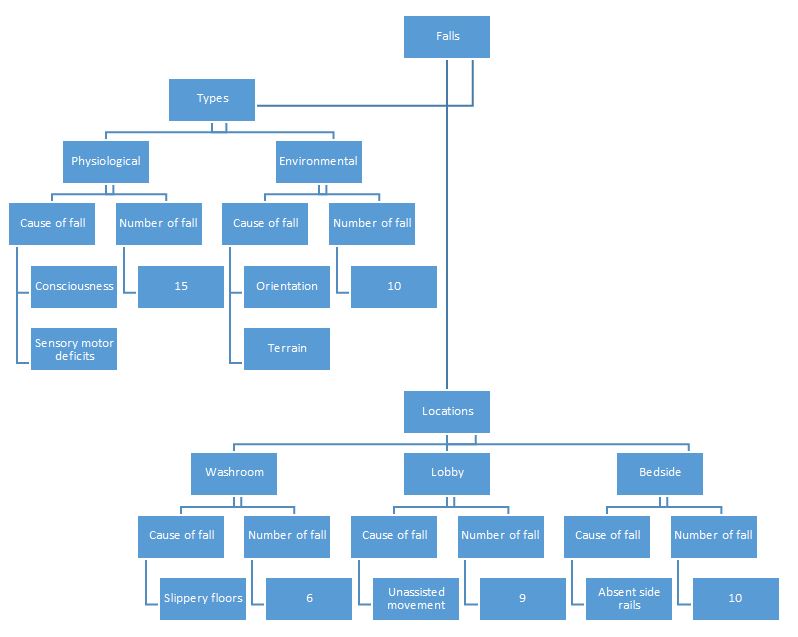
A Chart Showing the Fall Findings for the 30 Day Period
Possible Solutions to the Issue of Falls
Assessing all patients for risk of falls using a fall risk assessment score forms one of the key solutions to this problem. It will aid the nurses in identifying patients with a low, moderate, or high risk of falling. Therefore, if the assessment indicates that the patient is at higher risk of falling, the healthcare provider can recommend the necessary prescriptions to prevent further falls and reduce the chances of injury to the patient. Consequently, harmonizing collaboration between caregivers and patients to address the fall risk factors is crucial to controlling falls among patients (Rosen et al., 2018). Providers in collaboration with patients should investigate patients’ opinions of the causes of their falls and their readiness to change to lower the risk of falling again.
On the other hand, nurses should put assistive devices and commonly used items closer to the inpatients to allow them to access these devices quickly and safely. The items such as call bell, water, and Kleenex should be within immediate reach of the patients to avoid excessive reaching. This will significantly reduce and solve the issue of falls among patients. Education is also another critical solution to falls among patients. Physicians should give proper fall prevention strategies to both patients and their families to enable them to take precautions and necessary measures whenever the patient is exposed to the conditions of falling. Moreover, the falls caused by bed issues can be controlled by keeping beds in the lowest position for sedated, unconscious, or compromised patients. Furthermore, nurses should avoid using side rails when a patient is confused. Side rails may create a barrier that can be easily climbed and create a fall risk situation for dizzy patients. Similarly, the hospitals should ensure that the patients have proper footwear and mobility aids to prevent slips.
Finally, highlighting the relevance of strength and balance exercise in preventing falls among high-risk individuals is critical. The most effective single intervention for avoiding falls and fall-related injuries is exercise programs that focus on improving strength and balance. Older people do not engage in these types of workouts on a regular basis. And since other forms of exercise, such as stretching and walking, have not been demonstrated to minimize falls. Training must focus on increasing balance, be moderate to high in difficulty, and be practiced for a minimum of two hours per week to be effective. Caregivers can educate patients about fall prevention activities and connect them to relevant services such as physical therapists and community fall prevention programs to get started. It is critical to underline that the effects of exercise will not be obvious for several months and that practice must be continued to get the benefits. Evidence-based exercise programs can be delivered at home or as group classes in the community.
In conclusion, it is evident that falls among high-risk patients in surgical or medical wards constitute a significant issue in the United States. However, hospitals can significantly reduce falls through performance improvement teams. Measures such as risk assessment for patient falls, effective education, and collaboration between caregivers and patients, among others, are critical in reducing the number of falls. As a result, more study is needed to develop more advanced and realistic solutions to eliminate frequent falls.
Reference
Rosen, M. A., DiazGranados, D., Dietz, A. S., Benishek, L. E., Thompson, D., Pronovost, P. J., & Weaver, S. J. (2018). Teamwork in healthcare: Key discoveries enabling safer, high-quality care. American Psychologist, 73(4), 433. Web.