Introduction
Current evidence-based practices are very critical in determining the results of therapeutic, and behavioral interventions for patients with psychological problems. It is important to make the evaluation of evidence-based practices ubiquitous, and implement them effectively (Charles, 2001). Clinicians may meet their clients who present their issues, various symptoms, which involve a variety of complications. This perspective has been influenced by advanced education, training, economics, the setting in which the clinicians work, and individual experience. In this context, clinicians make assessments, diagnoses and make their decisions on the treatment of different patients.
This gives a reflection of the scientific evidence, and experience that comes from the encounters of patients with similar problems. Patients may decide to seek professional help from medical experts. They may also need to understand the diagnoses and the treatments, which they receive to cure their ailments. In this case, the paper provides a perspective of evaluating the current evidence-based procedures for individuals suffering from psychological problems (Miller, Wilbourne & Mesa, 2002).
Guidelines for Evidence-based Practices
Scientists have the ability to develop tests and implement interventions for different groups of clients by using evidence-based practices. This is based on the similarity of the symptoms, complains and history of the clients’ ailments. In this context, the effort to come up with reliable results may be guided by vigorous experimental, and scientific methods. This is meant to enhance the validity of the inferences concerning the results of the inventions, and assist in clinical (Marlatt & Gordon, 2000).
The virtue of using rigorous standard empirically, this type of evidence is less subjective to biases, it is objective and systematic in acquisition. More so, it appears in the increased objectivity in clinical research although there may be validity variations in the experimental design, assessments, methods of research and inclusion of the subject. Additionally, statistical processes are of great importance (Kathleen & Lisa, 2004).
Despite having scientific quality, a clinically researched and developed evidence-based intervention may be practically unfeasible since it is quite expensive, and complicated in relation to the focus on specific clients. According to Guyattt, clinical research annotations can be more systematic, and unassailable than the ones garnered through the insights of personal clinical, practitioners and their clients (Guyatt, et al., 2002).
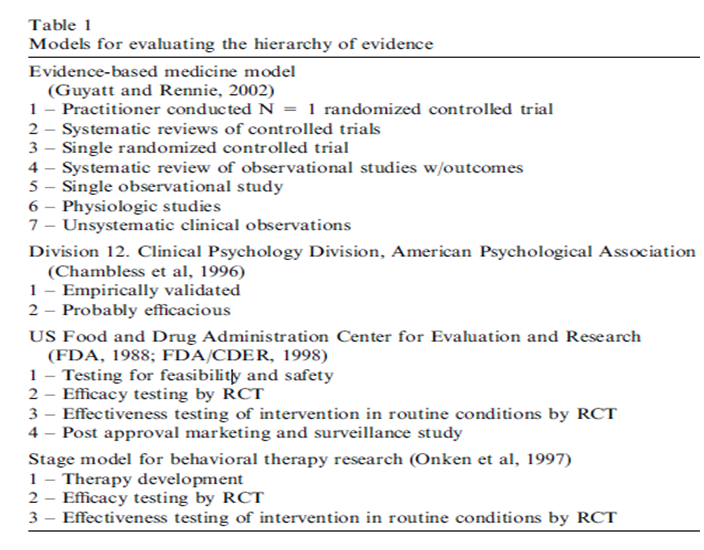
Clinicians and clients may have similar valid experiences with evidence-based practices. Clinical research may have an impact of providing this information in case scientific data fail to provide relevant, compelling results. The table below indicates guidelines and standards for current evidence-based practices along a hierarchy of potency of evidence ( Marlatt & Gordon, 2000). There are seven practices to confirm the validity of evidence-based practices. They include:
- Conducting a number of random trials with specific patients
- Systematic reviews of controlled trials
- Single random trials
- Systematic review of observational studies that address client results
- A single observational study that addresses important client’s outcome
- Physiologic studies that are best for medical practitioners as scientists
- Unsystematic clinical observations
The seven steps above can give the health practitioners the ability to identify the efficacy of a specific evidence-based practice. They can easily give better results for observing the data of a particular evidence-based practice.
References
Charles, P. O. (2001) A range of research-based pharmacotherapies for addiction. Web.
Guyatt, G, l. (2002). Introduction: the philosophy of evidence-based medicine. A manual for evidence-based clinical practice. American Medical Association. 3–12.
Kathleen, M. C and Lisa, S. O. (2007). Behavioral Therapies for Drug Abuse. Focus.Vol 2 (7), 5:240-248. Web.
Marlatt, G., and Gordon, J. (2000). Relapse prevention: maintenance strategies in the treatment of addictive behaviors. New York: Guilford.
Miller, W., Wilbourne, P and Mesa, G. (2002). A methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. New York: Guilford 97:265–77.