Tuberculosis is among the most infectious illnesses that affect the lungs. The disease spreads from one infected person to the next through its bacteria whenever tiny droplets are released when an individual sneezes or coughs. This bacteria is known as “Mycobacterium,” and its effects can spread to the spine and brains if not cured early enough (Churchyard et al., 2017). Moreover, different types of infection determine the nature and extent of the disease and the effectiveness of treatment. Nevertheless, this paper traces the history of this bacterial infection to date and looks at its statistical development in the South to evaluate its significance over time.
History of Tuberculosis
Ancient Times
Hypotheses hold that the “Mycobacterium” genus can be traced back to over 150 million years ago. Further, it is believed that one of the earliest progenitors of the Mountain Time (MT) brought the infection to East Africa and infected its early hominids (Barberis, Bragazzi, Galluzzo & Martini, 2017). Additionally, there is evidence that particular Egyptian mummies revealed certain deformities in their skeletal structure, which is a known symptom of Tuberculosis (Churchyard et al., 2017). Other documented records are related to Hebraism, suggesting that the infection was present long before the European pioneer colonized South America. Nonetheless, in Ancient Greece, the disease was referred to as Phthisis (Barberis et al., 2017). It was described as a fatal infection that mainly attacked young adults and was characterized by tubercular lung lesions (Churchyard et al., 2017). In Greece, promising discoveries about the disease were made, with Isocrates and Aristotle having records to suggest the infection’s nature (World Health Organization, 2017). Although TB might have been present during this time, it is unclear when it was discovered, as different people have different accounts of the bacterial infection.
Middle Ages
Around this time, a disease affecting the cervical lymph nodes, otherwise known as scrofula, was viewed to be the newest form of Tuberculosis and was even described in France and England as the “king’s evil.” Later in the 12th century, it was reported by William of Malmesbury that there were treatments for the infection, including royal tombs visits and coin-talisman (World Health Organization, 2017). Other scientists like Paul of Aegina and Guy de Chaulic also came up with their descriptions of the disease and proposed treatments based on their research and comprehension of its symptoms (Shrestha, Hill, Marks, & Dowdy, 2017). However, the infection’s detailed anatomical and pathological description was done in “Opera Medica” by Francis Sylvius in 1679 (World Health Organization, 2017). He described the infection’s progression, its tubercles, empyema, cavities, and its consumptive sites in patients. It is considered the first breakthrough in the identification of the disease.
The 18th and 19th Centuries
This is the period where most of the credible and reliable information about TB was coined. Benjamin Marten was able, for the very first time, to conjecture the origin of TB. Later in 1834, Johann Lukas Schonlein was the first to coin the term “tuberculosis,” as it had early been predominantly referred to as phthisis and consumption (Shrestha et al., 2017). The infection came to be considered an epidemic in Western Europe at about the same time due to its relatively high annual mortality rate of about 900 deaths per 100,000 inhabitants. In the 18th century, the disease was termed the “white plague” following its extreme anemic pallor.
At the beginning of the 19th century, debate arose due to the varied theories on the infection’s pathological origin. This was primarily caused by some considering it an infectious disease, while some saw it as a hereditary one. In 1810 and 1819, Gaspard-Laurent Bayle and Theophile Laennec’s made discoveries concerning the infection’s pathophysiology (Stewart, Tsang, Pratt, Price, & Langer, 2018). Several other theories followed until 1854, when Hermann Brehmer identified the first successful remedy. Later in 1867, Theodor Albrecht Edwin Klebs tried to isolate the infections bacillus (Barberis et al., 2017). However, it is Robert Koch who had a breakthrough in tubercle bacillus isolation. He announced his discovery of “Mycobacterium tuberculosis” on March 24, 1882, in Berlin to the Society of Physiology (Stewart et al., 2018). Decades later, Selman Waksman streptomycin, Pirquet and Mantoux tuberculin skin tests, Albert Calmette and Camille Guerin (BCG) vaccine, and other anti-tuberculous drugs were developed based on Koch’s milestone identification.
Tuberculosis Today
TB is among the leading causes of death, and it is the top for death from single infectious agents. The infection is present in all age groups and all countries, and in 2019 alone, it infected about ten million people (Eisinger, Embry, Read & Fauci, 2020). However, the infection’s incidence is higher in developing counties, mainly because of poor nutrition, improper sanitation, and co-infection with human immunodeficiency virus (HIV) (Fojo et al., 2017). For this reason, there is a combined strategy involving drug treatment improvement, prevention, and diagnostic instruments in place (Eisinger et al., 2020). The World Health Organization (WHO) believes that through this perfect mix, “Mycobacterium tuberculosis” will be eradicated by 2050.
Tuberculosis in South Carolina
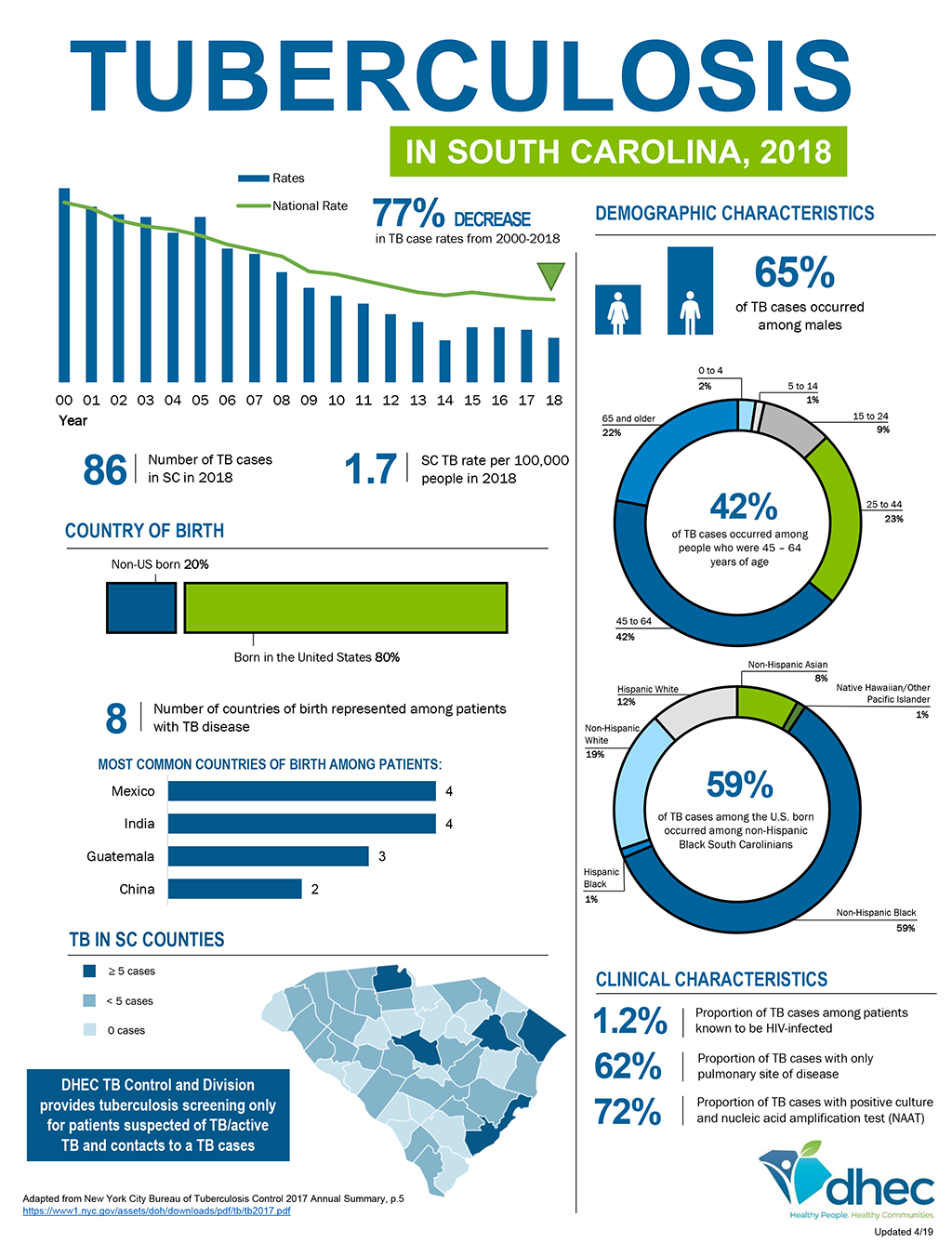
Tuberculosis cases have been on a downward trend in South Carolina since 1980. However, around 1985, cases increased within the state due to a rise in ethnic minorities (“TB data & statistics,” 2019). Additionally, there was widespread HIV infection wherein most of those infected with the virus were co-infected with the bacterial infection (Lewinsohn et al., 2017). This led to the strengthening and revamping of TB control programs, and the rates have been on a downward trend since.
Significance of Decrease
Before the 1980s, tuberculosis cases in South Carolina were relatively higher. However, the rates became relatively static in the early 1980s. However, from around 1986, the rates have been decreasing to date. Both high and rural poverty state areas have continued to experience significant infection incidence changes (“TB data & statistics,” 2019). This decrease is essential because it has led to increased life expectancy in the state. Moreover, these numbers reflect the milestones made in discovering a treatment for this infection and the increase in awareness of how to handle those who are infected (Jo, 2017). Furthermore, it is a powerful depiction of the state’s steps towards achieving quality healthcare, considering that TB is still among the top causes of death worldwide.
The numbers are primarily low because of the state’s unique approach to the disease. South Carolina has a unique tuberculosis control program that incorporates statewide enablers, directly observed therapy, and incentives that ensure that diagnosis and treatment are fast enough (Lewinsohn et al., 2017). Moreover, it has invested heavily in case finding, treatment of latent and active Tuberculosis, targeted evaluation of those most susceptible to the infection, and testing and identifying those exposed (Jo, 2017). The services within this coordinated approach include public health clinics, case management, radiology, physician services, medications, and outpatient hospital services (Fojo et al., 2017). With such an approach, the state is on its way to eliminating TB within its boundaries.
Conclusion
Tuberculosis has claimed millions of lives globally to date. However, research and advancements in science have enabled scientists to develop better ways of diagnosis and treatment. However, the infection still lives, and even with its reduced incidence, it claims several lives annually (Jo, 2017). Governments must prioritize preventive mechanisms to handle the disease’s spread to ensure that everyone stays safe from the condition. Therefore, it is vital to continue creating awareness of some of these mechanisms to ensure that individuals protect themselves and those around them.
References
Barberis, I., Bragazzi, N., Galluzzo, L., & Martini, M. (2017). The history of tuberculosis: From the first historical records to the isolation of Koch’s bacillus. Journal of Preventive Medicine and Hygiene, 58(1), 9-12.
Churchyard, G., Kim, P., Shah, N., Rustomjee, R., Gandhi, N., & Mathema, B. (2017). What we know about tuberculosis transmission: An overview. The Journal of Infectious Diseases, 216(6), 629-635.
Eisinger, R., Embry, A., Read, S., & Fauci, A. (2020). 2019: A banner year for tuberculosis research. The Journal of Infectious Diseases, 222(11), 1768-1771.
Fojo, A., Stennis, N., Azman, A., Kendall, E., Shrestha, S., Ahuja, S., & Dowdy, D. (2017). Current and future trends in tuberculosis incidence in New York City: A dynamic modelling analysis. The Lancet Public Health, 2(7), 323-330.
Jo, K. (2017). Preventing the transmission of tuberculosis in health care settings: Administrative control. Tuberculosis and Respiratory Diseases, 80(1), 21.
Lewinsohn, D. M., Leonard, M. K., LoBue, P. A., Cohn, D. L., Daley, C. L., Desmond, E., & Woods, G. L. (2017). Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention clinical practice guidelines: Diagnosis of tuberculosis in adults and children. Clinical Infectious Diseases, 64(2), 111-115. Web.
Shrestha, S., Hill, A. N., Marks, S. M., & Dowdy, D. W. (2017). Comparing drivers and dynamics of tuberculosis in California, Florida, New York, and Texas. American Journal of Respiratory and Critical Care Medicine, 196(8), 1050-1059.
Stewart, R. J., Tsang, C. A., Pratt, R. H., Price, S. F., & Langer, A. J. (2018). Tuberculosis – United States, 2017. Morbidity and Mortality Weekly Report, 67, 317-323. Web.
TB Data & Statistics. (2019). Web.
World Health Organization. (2017). Ethics guidance for the implementation of the End TB strategy. Web.