Introduction
The subsequent discussion focuses on the connection between hypertension and kidney disease. It will also discuss why controlling blood pressure (BP) is a requisite aspect in slowing the advancement of renal damage. Many Chronic Kidney Disease (CKD) patients struggle with hypertension. High blood pressure (HBP) eventually deteriorates human health since it causes cardiovascular diseases and other complications. Thus, if blood pressure can be controlled, then renal disease can be managed effectively.
Overview of Kidney Disease
Kidney disease is a global public health menace. A 2009-10 report by the National Health Service (NHS) Kidney Care has revealed that chronic kidney disease costs the NHS up to £1.45 billion pounds in a year. In the US, the situation is exacerbated by the fact that most patients are undiagnosed and/or do not receive proper treatment. CKD is linked to increased cardiovascular indisposition and mortality Hence, physicians can effectively manage CKD not only by focusing on treating it but also preventing and controlling risk factors that are associated with CKD.

Hypertension/HBP and Kidney Disease
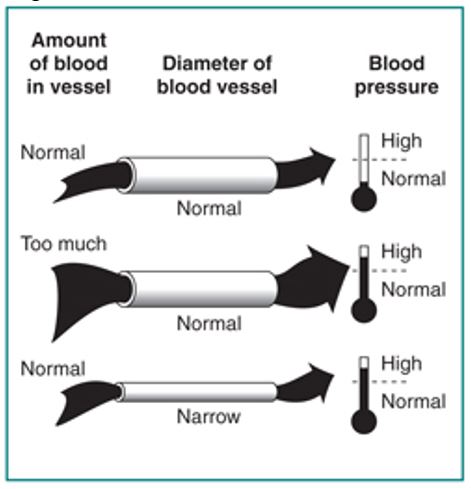
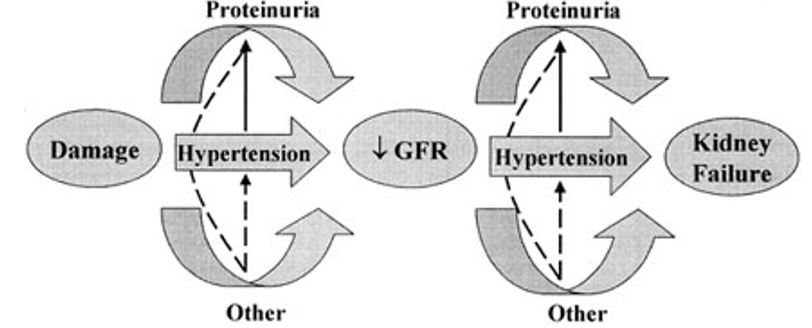
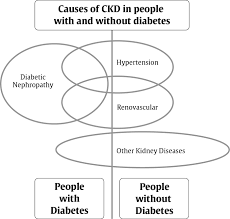
Blood pressure refers to the force that emanates as blood is transported from the heart to the other parts of the body. Hypertension refers to a rise in the force of blood moving from the heart above the expected pressure. This elevated pressure is caused by increased volume of blood because of additional fluids or constricted blood vessels. Often, HBP is either is a source or a result of CKD (Hunt 2011). Hypertension may rise in the development of CKD and can be detected through deteriorating kidney performance as well as the rise of heart disease. It is a key agent for the decrease in glomerular filtration rate (GFR) not only in diabetic renal disease but also non-diabetic patients. GFR refers to the test that evaluates the performance of kidneys.
The systemic blood pressure capacity is a key HBP-linked element that contributes to the destruction of the kidney. When the kidney is healthy, the renal blood flow (RBF) barely changes within a wide range of mean arterial pressure (MAP) that is, between 80 and 160 mmHg. As the blood pressure rises within this range, vasoconstriction of the glomerular vessel makes the pressure stable. As a defensive development, chronic HBP normally distorts the renal blood flow ((Bomback, Kshirsagar, & Amamoo 2008). The increased force of blood flow to the renal vasculature causes an automatic expansion of the glomerular capillaries as well as mesangial cells.
HBP accelerates the exacerbation of kidney disease by facilitating glomerular injury. The proteinuria aggravates the condition as injures the kidney vessels. The destruction of renal vessels interferes with the kidney to achieve its role (Sarafidis & Ruilope 2011).
Renal disease does not exhibit any symptoms during the initial stages
Fortunately, as the ailment advances, various symptoms such as nausea, dry skin, and vomiting. If hypertension can be diagnosed promptly, then physicians can easily manage CKD through proper management. Management should focus on establishing optimal blood pressure. This target may, however, vary depending on whether one is diabetic or not (Hackam, Quinn, & Ravani 2013).
Blood pressure control in non-diabetic kidney disease patients
The Modification of Diet in Renal Disease (MDRD) research is the first study to investigate the impact of lowering the BP target to alter the progress of kidney disease (Ruggenenti, Perna, & Loriga 2005). Diabetic individuals under insulin medication did not participate in the research except for 26 individuals with diabetic nephropathy. During the period of the study, the mortality rate of renal disease reduced considerably. Moreover, the number of patients who got to ESRD level declined. The study showed that low BP goal is effective in managing renal disease among proteinuric individuals (Lewis & Noble 2012).
Another important investigation was the African-American Study on Kidney Disease (AASK). It addressed some limitations that had been witnessed in the initial study. The results of both studies revealed that lowering the blood pressure was effective in altering the development of kidney disease over prolonged time. Nonetheless, MDRD and AASK studies retrieved their facts from sub-group assessments or randomised stages with long-standing observations (McCormick, Hiremath, & Ruzicka 2014). However, in both studies, the MAP degrees were unsystematic with respect to the patients systolic and diastolic blood pressure. Consequently, there is the need for the future researchers to consider the existing loopholes in the studies to provide a better evidence-based blood pressure control formula for non-diabetic kidney disease patients. Meanwhile, a target of <130/80 as suggested in the AASK research would be the most preferable particularly for individuals with urine protein secretion over 0.25-0.3. gr/day (Ruggenenti, Perna, & Loriga 2005).
According to Sarafidis and Ruilope (2011), while several studies determine the optimal blood pressure that limit the growth of renal disease, there is still no adequate evidence-based tactic for setting blood pressure goals for diabetic CKD patients. Initially, unsystematic assessment on diabetic individuals who had differing points of kidney performance as well as albumin secretion that likened various blood pressure targets did not disclose any notable differences in creatinine reduction. Instead, there was a decline of proteinuria coupled with gradual advancement to macroalbuminiria. Minimising spontaneous bacterial peritonitis (SBP) to 130 mmHg has the potential to reduce GFR.
Clinicians continue to use evidence-based approach for controlling blood pressure among diabetic renal disease patients. However, the existing guidelines recommend setting a goal of the <130/80 mmHg for victims with diabetes (Becker, Hewitson & Chrysostomou 2009). For patients with type 2 diabetes, clinicians observe that antihypertensive therapy and ACEi help in disrupting the growth of albuminuria and relapse of normoalbuminuria (Sarafidis & Ruilope 2011).
Lifestyle and Drug Therapy for reducing blood pressure among renal disease patients
Blood pressure can be reduced using both pharmacological treatments and lifestyle adjustments (McCormick, Hiremath, & Ruzicka 2014). However, achieving a blood pressure reduction is often difficult for senior patients, diabetes mellitus patients, as well as those with co-morbidities. The reason is because of the elevated conduit-artery constriction. Senior CKD patients and victims of diabetes are susceptible to orthostatic hypotension, a situation that is worsened by volume reduction (Goodfriend 2007). Most CKD patients should be given medications that can regulate blood pressure particularly, vasodilators. However, it is important to constantly check for the side effects, which include vertigo and postural hypotension.
Numerous evidence-approaches can effectively assist a CKD patient to establish an optimal blood pressure target (Hackam, Quinn, & Ravani 2013). Observational assessments have associated factors such as salt intake, weight-reducing diet and consistent workout. Lifestyle therapy is a more convenient and cheap means for kidney disease patient to regulate their blood pressure levels. It offers the patients an opportunity to improve the performance of other body organs such as the liver (Ruggenenti, Perna, & Loriga 2005).
Undergoing a programme for reducing weight is generally seen to lower blood pressure to the desired levels. Taking particular diet can help a kidney disease patient to shade weight and minimise release of urinary protein. Lowering salt intake is also a good step towards blood pressure reduction. Individuals who struggle with CKD can significantly drop urine albumin by lowering the content of sodium in their meals. Some types of renal diseases can be linked with reduction of salt in the kidney.
People with the mentioned condition are likely to struggle with volume diminution as well as electrolyte disorders. As such, it is important to monitor the conditions volume and electrolyte for patients undergoing salt intake regulation. Similarly, minimising alcohol intake is also vital for individuals who to create an optimal blood pressure (Lewis & Noble 2012).
Conclusion
Taking a standard drink, about 19.7 of alcohol, can help to regulate the level of blood pressure. This restraint in alcohol consumption should be closely followed by avoiding smoking tobacco. The chemicals in cigarettes heighten instances of heart and kidney diseases. However, no adequate evidence shows a direct impact of tobacco smoking on blood pressure (Schneider & Hilgers 2014). Management of blood pressure to an optimal standard is one of the key ways of limiting the progression of kidney disease. Nevertheless, the controlling blood pressure can only be successful if evidence-based methods are utilised. Currently, the literature on kidney disease, hypertension, and diabetes and their connection is still developing.
References
Becker, J, Hewitson D & Chrysostomou, A 2009, ‘Aldosterone in clinical nephrology–old hormone, new questions’, Nephrol Dial Transplant, vol. 24, no. 1, pp. 2316–2321.
Bomback, S, Kshirsagar, V & Amamoo, A 2008, ‘Change in proteinuria after adding aldosterone blockers to ACE inhibitors or angiotensin receptor blockers in CKD: a systematic review’, Am J Kidney Dis, vol. 51, no. 2, pp. 199–211.
Goodfriend, L 2007, ‘Treating resistant hypertension with a neglected old drug’ Hypertension, vol. 49, no. 3, pp. 763–764.
Hackam, G, Quinn, R & Ravani P 2013, ‘The 2013 Canadian Hypertension Education Programme recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension’, Can J Cardiol, vol. 29, no. 2, pp. 528–542.
Hunt, A 2011, Kidney Disease: A Guide for Living, John Hopkins University Press, Maryland.
Lewis, R & Noble, H 2012, Kidney Disease Management: A Practical Approach for the Non-Specialist Healthcare Practitioner, John Wiley & Sons, New Jersey.
McCormick, B, Hiremath, S & Ruzicka, M 2014, ‘Lower blood pressure target in nondiabetic proteinuric chronic kidney disease is not justified’, Kidney International, vol. 86, no. 1, pp.855-855.
Ruggenenti, P, Perna, A & Loriga, G 2005, ‘Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial’, Lancet, vol. 365, no. 2, pp. 939–946.
Sarafidis, A & Ruilope, L 2011, ‘Aggressive blood pressure reduction and renin-angiotensin system blockade in chronic kidney disease: time for re-evaluation?’, Kidney Int, vol. 85, no. 1, pp. 536–546.
Schneider, M & Hilgers, K 2014, ‘What should be the goal blood pressure in nondiabetic chronic kidney disease?’, Curr Opin Nephrol Hypertens, vol. 23, no. 2, pp. 180-185.