Boston Medical Center is a large-scale non-profit 514 bed urban hospital located in Boston, MA. It is considered the largest safety-net hospital as well as a level-1 trauma center in all of New England. Despite its reputable facilities and high-level expertise, the hospital has faced a significant organizational problem. The issue is patient identification in the EHR. Patient identity and patient record matching is a critical topic and foundation for modern electronic records. Patient matching consists of identification of the patient and linking the patient’s data across health systems to obtain a comprehensive healthcare record while also providing accurate service (HealthIt.gov). Some examples of patient identification errors are:
- The wrong diagnostic test done because of patients sharing similar names;
- Mix-up in CT scans in similar patients sharing neighboring rooms;
- A patient has a wrong identification badge, potentially receiving the wrong medicine;
- During new patient admission, the EHR identifies a patient as someone else, resulting in a wrongful insurance claim.
Patient identification is a significant patient safety issue as inaccurate EHR data, lack of confirmation of identity, and human or technological errors can result in wrongful treatments, procedures, testing, and further healthcare decision-making that has a high potential of placing the patient in danger. Further organizational challenges can stem from inaccurate identification, include miscommunication among departments, ineffective treatment provided, and issues with data and billing. Due to safety concerns and obvious failure to provide competent medical service in cases of patient identification errors, this becomes both a quality and regulatory issue.
The reported industry standard for patient identification errors is 8-10%, but a 2016 comprehensive National Patient Misidentification Report found that in more half of healthcare organizations across the country, the errors happen more frequently than reported. Another analysis from the Veterans Health Administration found that 182 of 253 errors in the test cycle are due to patient misidentification. On average, a hospital loses $17.4 million annually because of patient misidentification, largely from denied insurance claims (Choudhury & Vu, 2020).
The patient identification issue is common around the world, so various solutions have been introduced to address it. One of the most common solutions, utilized in the health systems of multiple EU and other developed states, is unique patient identifiers (UPIs). These essentially assigned a national identified number to every patient in the system, eliminating the need to rely on patient attributes for matching. However, in the United States, the adoption of UPIs was shut down in 1996 due to privacy and security concerns (Riplinger et al., 2020).
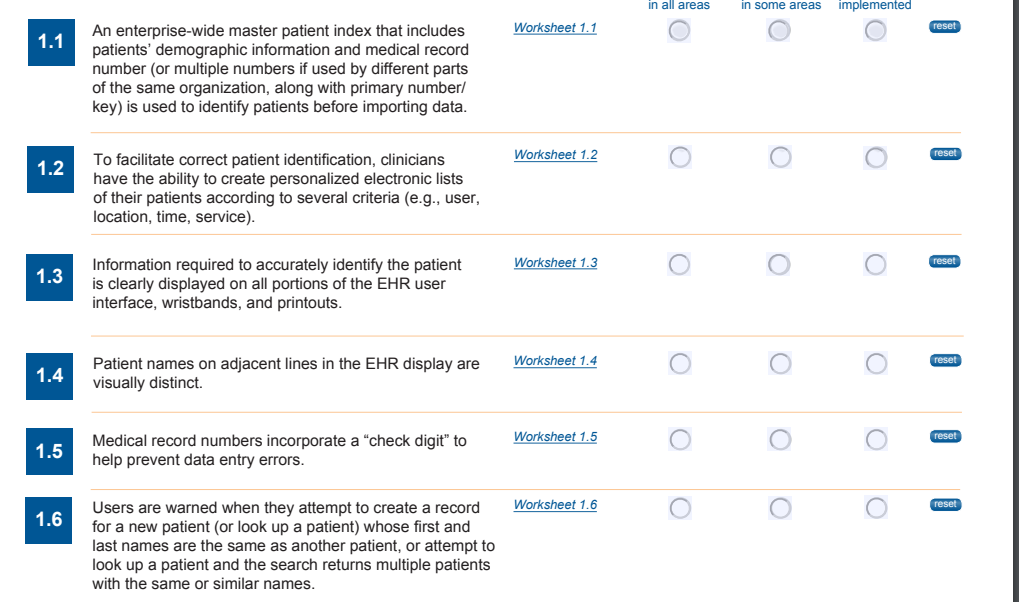
The Office of the National Coordinator for Health Information Technology (2016) has released Safety Assurance Factors for EHR Resilience (SAFER) aimed at regulating and guiding health care organizations to optimize for safe use of electronic health records. SAFER specifically outlines patient identification as one of the key 8 factors that necessary for reliable safety practice to ensure that the information presented by the EHR or entered into the system represent the correct person being treated. There are several points of potential breakdowns where patient identification errors can occur from both human and technological perspectives. SAFER has created a multi-point checklist which organizations, employees, as well as other stakeholders (such as EHR developers) can follow to ensure better patient identification accuracy.
The various measures and techniques seen in Figure 1 below act as redundancy methods to ensure the accurate verification of the patient’s identity. Furthermore, the Joint Commission accreditation organization requires the use of two patient identifiers prior to providing care. They suggest that identifiers such as name, assigned identification number, telephone, or other unique personal identifiers are appropriate. The use of a medical record number or electronic identification technology such as bar coding or RFID are appropriate if including two or more person-specific identifiers (The Joint Commission, n.d.).
References
Choudhury, L.S., & Vu, C.T. (2020). Patient identification errors: A systems challenge. Web.
HealthIt.gov. (n.d.). Patient identity and patient record matching. Web.
Riplinger, L., Piera-Jiménez, J., & Dooling, J. P. (2020). Patient identification techniques – Approaches, implications, and findings. Yearbook of Medical Informatics, 29(1), 81–86. Web.
The Joint Commission. (n.d.). What are the key elements organizations need to understand regarding the use of two patient identifiers prior to providing care, treatment or services? Web.
The Office of the National Coordinator for Health Information Technology. (2016). Self-assessment: Patient identification. Web.