The problem: Lack of Connectivity between Healthcare Services and Patients without Insurance
Background: Affordable Care Act and Its Effects
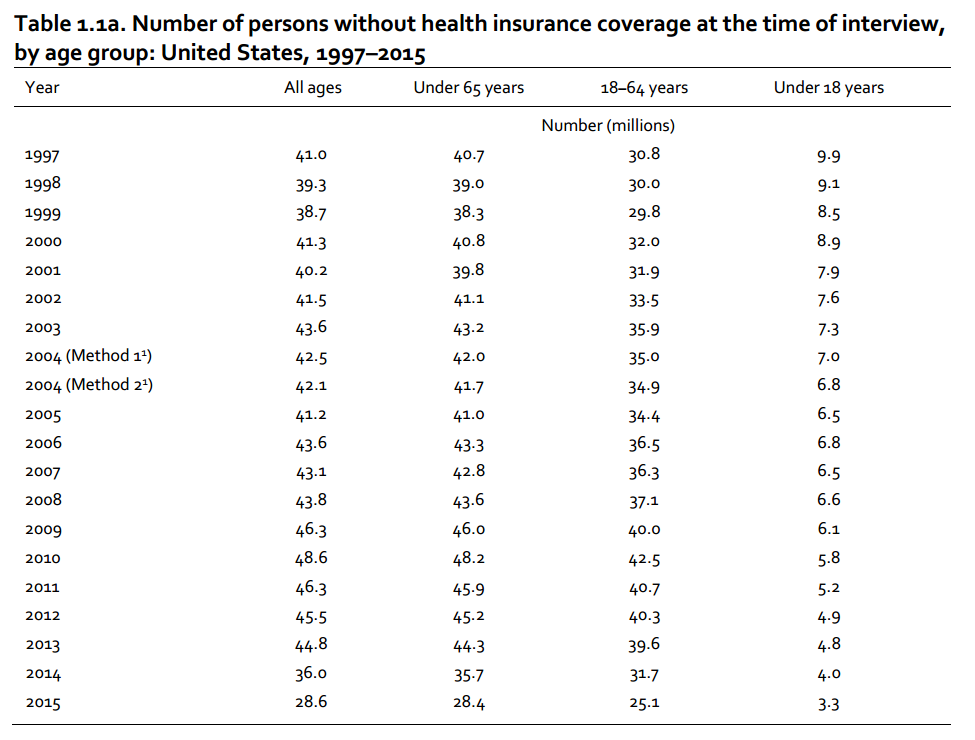
With the adoption of the Affordable Care Act (ACA), a significant improvement in the accessibility of healthcare services to the general U.S. population was expected, yet the hopes of the U.S. government and the target population were proven mostly wrong (Beck et al., 2014). According to the current statistics, in 2015, 4.5% of people could not receive the required healthcare services because of their high cost (Centers for Disease Control and Prevention, 2016). Even though there seems to be a tendency toward a gradual drop in the number of people that do not have access to the subject matter, the problem remains huge (see Fig. 1).
Therefore, the effects of ACA are dubious at best. The reason for the identified problem exist is the lack of connectivity between the target residents of U.S. communities and the corresponding healthcare facilities (Anderson, Davidson, & Baumeister, 2013). As a result, while the levels of healthcare affordability are slowly increasing, a number of people remain helpless and unprotected from the threats to their health.
Significance: Disease Prevention and Management as a Priority
Given the fact that a significant number of U.S. citizens still do not have access to healthcare services, it is crucial to explore the opportunities for addressing the situation accordingly. To improve health outcomes in the target population, one must reconsider the current approach toward information management and communication in healthcare. Particularly, it is crucial to make sure that the people that are unable to receive the relevant healthcare services should be given a chance to engage in successful self-management and receive guidance from the local healthcare services. Therefore, it is essential to explore the options for promoting reciprocity between healthcare organizations and patients that do not have the opportunity to receive the required services (Buchanan et al., 2013).
Therefore, it can be assumed that the significance of the study is rather high. The outcomes of the research will provide the foundation for developing a program that will, later on, serve as the tool for improving patient outcomes. Consequently, a steep rise in the accessibility of healthcare services for patients with low income can be expected with the adoption of the said programs.
Research Questions, Hypothesis, and Variables with Operational Definitions
Research Question: Determining the Focus of the Study
It is crucial to make sure that the patients from low-income families, as well as other disadvantaged members of the American population that currently do not have access to healthcare services, should be provided with an opportunity to receive the minimum of the required care. The tools such as self-management and consistent knowledge acquisition by means of maintaining a dialogue with healthcare facilities are viewed as a possible solution. Therefore, the study in question will seek to answer the following question:
“Does the promotion of self-management and the emphasis on enhancing the communication between the people that do not have access to healthcare and the corresponding healthcare organizations allow for the increase in positive health outcomes in the identified population?”
In other words, the study will focus on exploring the effects that self-management strategies have on people’s health. Furthermore, the significance of communication between healthcare organizations and the members of the community who do not have access to the services will be evaluated. Thus, the foundation for building an efficient program will be provided.
Hypotheses: Assumptions about the Efficacy of Self-Management and Communication
- Hypothesis A. The success of self-management strategies adoption among and the establishment of a coherent and consistent dialogue between the members of the U.S. population that do not have access to healthcare due to low income or other impediments is in direct proportion to the positive outcomes among the identified population.
- Null Hypothesis. There is no correlation between the use of the programs aimed at encouraging self-management, the establishment of a dialogue between patients with low income and the healthcare facilities, and the increase in positive outcomes among the identified members of the U.S. population.
Operationalizing Variables: Relationships between the Key Phenomena of the Study
The changes in the positive patient outcomes among the members of the U.S. community that do not have access to healthcare services will be viewed as the key dependent variable. The percentage of the members of the financially disadvantaged population that will show positive patient results will be calculated so that the differences between the previous approaches and the suggested one could be determined.
The strategies based on the promotion of self-management and the establishment of a dialogue between the members of the U.S. population that cannot get access to healthcare services will, in turn, be the primary independent variables that will ostensibly contribute to an increase in positive patient outcomes. The efficacy of the promotion process will be based on the percentage of the population that will be provided with the relevant information and the tools for successful self-management.
References
Anderson, R. M., Davidson, P. L., & Baumeister, S. E. (2013). Improving access to care. In G. F. Kominski, Changing the U.S. health care system: Key issues in health services policy and management (4th ed.) (pp. 93-129). New York, NY: Jossey-Bass.
Beck, E., Craig, A., Beeson, J., Bourn, S., Goodloe, J., Moy, H. P.,… White, L. (2014). Mobile integrated healthcare practice: A healthcare delivery strategy to improve access, outcomes, and value. Web.
Buchanan, N., King, J. B., Rodriguez, J. L., White, A., Trivers, K. F., Forsythe,… Sabatino, S. A. (2013). Changes among US cancer survivors: Comparing demographic, diagnostic, and health care findings from the 1992 and 2010 national health interview surveys. Oncology, 2013(238017), 1-9. Web.
Centers for Disease Control and Prevention. (2016). Early release of selected estimates based on data from the 2015 National Health Interview Survey. Web.