Abstract
Type 2 diabetes is a crucial health issue that cannot be ignored due to the numerous risk factors that are associated with the given condition. The case of MG shows that there is a rather thin line between a healthy individual and a patient with a distinguishable case of diabetes. MG’s parents suffer from heart diseases and diabetes that have been caused by excessive body weight and an incorrect lifestyle. It may be safe to say that the current case represents an accurate depiction of what might occur when one disregards evident health issues and chooses to introduce no changes to their daily food consumption. Based on the information collected during a detailed review of systems, it was proposed to mediate weight-gaining activities and come up with strategies for generating more physical activity. It is also possible that MG’s child is going to require a similar treatment because his symptoms are similar to those of the father.
History
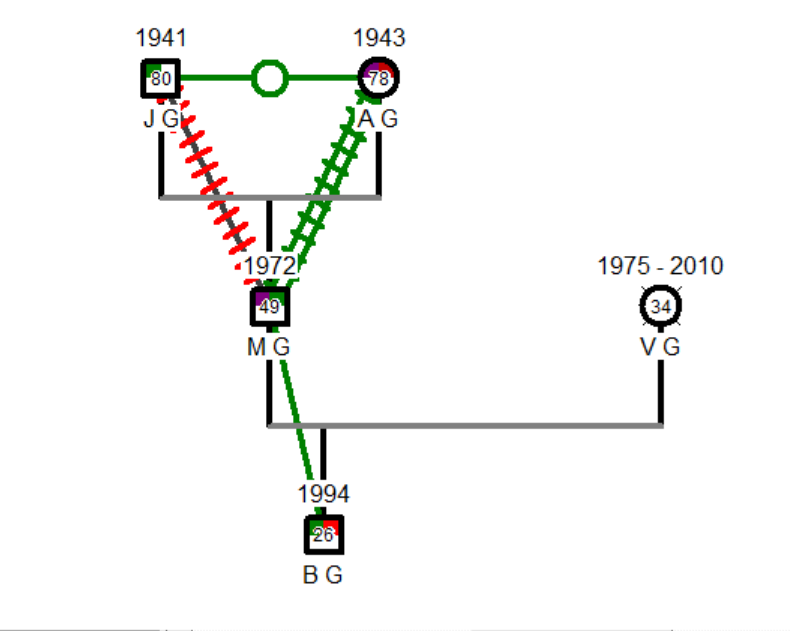
The patient (MG) is a 49-year-old Caucasian male of Italian descent. He has both parents (JG and AG) and a 26-year-old son (BG). A thorough interview with MG showed that he rarely speaks to his parents due to the problems related to his marriage and the death of his wife, VG. No specific problems or concerns associated with medications, immunizations, or allergies have been found throughout the examination. Despite being a widower, MG has an exceptionally positive relationship with his son (see Figure 1). Both MG’s parents and the child are exposed to diabetes and overweight. The chief concern mentioned by the patient was the presence of worsening diabetes symptoms that affect MG’s quality of life and make it harder for him to sustain a persistent lifestyle. There were no particular issues linked to the patient’s dental history either.
Review of Systems
- General constitutional symptoms: The patient does not experience night sweats or fevers. A slight weight change occurred within the past six months. The patient suffers from fatigue rather often despite being relatively used to physical exercise.
- Skin, hair, & nails: No evident skin lesions were identified, but some of the patient’s body areas became darker.
- Head & neck: Abnormalities related to the development of MG’s head and neck have not been identified.
- Eyes: MG does not seem to experience any vision changes since his last visit to the doctor. No redness, eye pain, discharges, or foreign bodies have been identified. Nevertheless, the patient remembered that his vision gets a bit blurry from time to time.
- Ears, Nose, Throat & Mouth: The patient hears well and does not indicate any specific changes or pains related to his ears. Nasal congestion is absent, and sinus pains were not found in MG either. The patient does not mention swallowing difficulties or having a sore throat.
- Chest & lungs: MG does not smoke, just like all the remaining members of his family. No signs of cough or wheezing have been identified during the evaluation.
- Heart and blood vessels, peripheral vasculature: There were no chest pains mentioned by the patient, with no palpitations or dyspnea.
- Lymphatic, hematologic: The patient does not experience any occasional bleeding, there is no history of transfusions, and it is relatively hard to bruise his skin. Speaking of MG’s endocrine system, no temperature intolerance or polydipsia/polyuria have been identified.
- Gastrointestinal: MG does not report any pains related to the gastrointestinal area since there have been no cases of vomiting, nausea, constipation, or diarrhea. He is not anorexic or excessively overweight, with no jaundice or flatulence identified either.
- Genitourinary: The patient does not experience any specific changes in the urinary flow and continence. There are no signs of dyspareunia and dysmenorrhea in the patient.
- Musculoskeletal: MG does not provide any information about injuries or past back and neck pains. Joint swelling and stiffness could not be found, hinting at a decent musculoskeletal development and absence of myalgias and arthralgias.
- Neurological: MG has never experienced a loss of consciousness in his life. There were no recent falls that could contribute to a worse health condition. There is occasional dizziness reported by the patient, but it does not get followed up by numbness or weakness.
- Mental health: There are no social issues or personality changes that could affect MG’s life or relationships with other people. He does not report insomnia, depression, memory loss, or a history of family abuse or violence.
Additional Review
The functional assessment of MG did not show any specific health challenges or obstacles to the proposed treatments for the patient’s type 2 diabetes. The patient’s muscles are strong enough to help him maintain an active lifestyle and occasionally appeal to physical exercise. The mini-cog assessment did not highlight any cognitive impairments that could avert MG from requesting relevant treatment for his type 2 diabetes and engaging in all the required activities.
Problem List
The key health problem that was identified is the presence of a quickly developing diabetes type 2 condition that has to be slowed down and mitigated with the help of a complex treatment plan.
The key health promotion areas that have to be touched upon by the care providers are a decent diet and the popularization of physical exercise intended to help MG lose weight and focus on both his mental and physical state.
NANDA Diagnosis and Treatment Planning
Diagnosis
MG does not adhere to any specific diabetes management plans at the moment, which forces his type 2 diabetes to develop at a rather high pace, causing an inadequate shift of blood glucose. The patient does not possess enough information on the topic of mitigating type 2 diabetes as well. Therefore, further planning should include interventions that close all the gaps and remove essential deficiencies.
SMART Objectives
- SO1: Test MG’s blood sugar once a week in order to see treatment dynamics and introduce quantitative changes to attain a positive change within the next three months.
- SO2: Work together with a nutritionist to provide the patient with an opportunity to lose 10 pounds over the course of the next four months.
Collaborative Interventions
The first iteration of the care plan will be the implementation of a detailed schedule including a variety of physical activities. MG will benefit from this proposal due to his willingness to regulate blood sugar levels. There are several options that the patient could choose from, such as aerobics and resistance exercise (Magkos et al., 2020; Taylor, 2020). An essential task for MG will be to avoid remaining inactive for more than three days in a row because even light activity brings more positive change than cognizant idleness. Overall, the idea with this segment of the care plan is to make sure that MG realizes the need to change his lifestyle and engage in more physically rewarding activities.
Another part of the care plan is to motivate the patient to lose some weight in an attempt to lower blood pressure, sugar level, and cholesterol. The fact that MG is overweight makes it safe to say that a customized diet could become an effective way of managing type 2 diabetes (Chopra, 2018). When monitoring blood sugar, the patient will meet the target range more often and avoid situations where his condition might get worse without other people knowing about it. The advent of numerous technologies makes it easier for both patients and providers to communicate in real-time with no delays.
References
Chopra, H. K. (2018). Cardiodiabetes update: A textbook of cardiology. JP Medical Ltd.
Magkos, F., Hjorth, M. F., & Astrup, A. (2020). Diet and exercise in the prevention and treatment of type 2 diabetes mellitus. Nature Reviews Endocrinology, 16(10), 545-555.
Taylor, R. (2020). Life without diabetes: The definitive guide to understanding and reversing type 2 diabetes. Simon and Schuster.